Introduction
Reactive arthritis (ReA) originally described as a triad of arthritis, conjunctivitis and urethritis is an immune response to bacterial infections of the gastrointestinal tract (GIT) and the genitourinary system especially in human leukocyte antigen (HLA)-B27 carriers.1–3 The ocular manifestations of ReA typically include conjunctivitis, iritis and uveitis.4 Keratitis denotes inflammation of the cornea, and it can microbial or non-microbial. In ReA, the spectrum of keratitis has been described from mild pleomorphic stromal keratitis to corneal ulcers.4–11 Keratitis in ReA is rare and mostly manifests as a mild pleomorphic anterior stromal keratitis seen in young men,4–8 with corneal ulcers being distinctly rare.7,10 We present here the case of a corneal ulcer as an ocular manifestation of ReA.
Case presentation
A 20-year-old man presented with a two-week history of pain and swelling of both knees and ankles, so severe he could not walk and had to be carried to the emergency room. There was pain over the left iliac crest, both shoulder tips and costochondral junctions, increasing on inspiration indicating enthesitis. He gave a history of diarrhoea about four weeks earlier which was associated with fever. The diarrhoea resolved, but the fever persisted for a few days before the onset of the arthritis. There was also history of redness of both eyes two weeks before, which resolved spontaneously. There was no history of oral or genital ulcers, skin rash, sore throat, ongoing fever or leg ulcers. On examination, there was swelling and tenderness of the right ankle, knee (Figures 1A and B) and first metacarpophalangeal joints. The left ankle, knee and both shoulders were tender. Vitals signs and systemic examination was within normal limits.
Figure 1 Clinical photograph showing swelling of right ankle (A) and both knees (B). Slit lamp photograph showing 3 × 4 mm oval paracentral corneal ulcer with underlying dense stromal infiltrates at presentation (C). OD, right eye oculus dexter
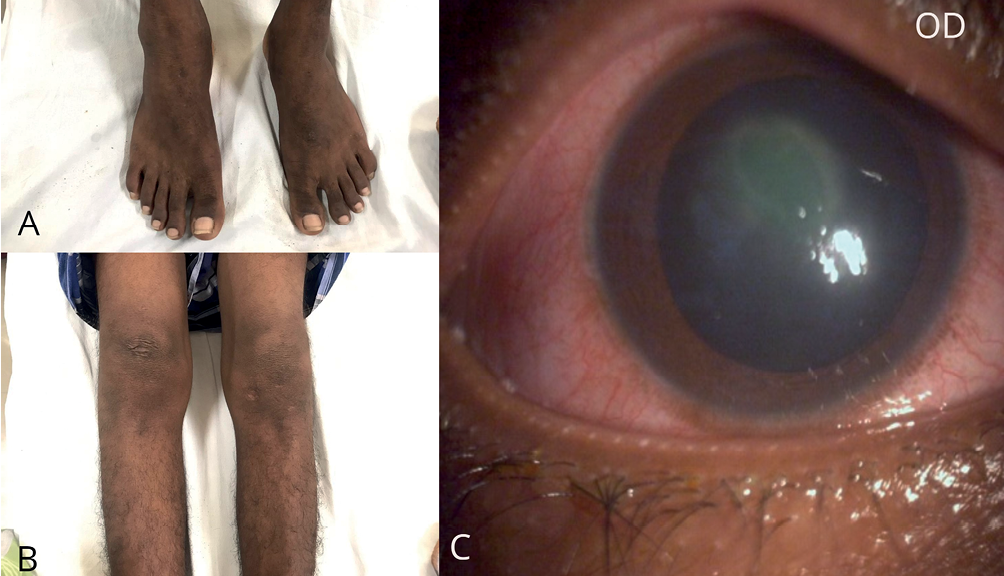
Disseminated gonococcal infection was considered as a differential diagnosis, hence blood and urine cultures were taken and he was started on intravenous ceftriaxone. Acute rheumatic fever was ruled out by a normal echocardiography and normal anti-streptolysin antibodies. In view of lower limb predominant arthritis, enthesitis and preceding GIT infection, acute ReA was also considered and he was given non-steroidal anti-inflammatory drugs (NSAIDs). He did not respond adequately to NSAIDS, hence synovial fluid analysis was performed which showed an inflammatory picture with absent crystals. Cultures of blood, urine and synovial fluid were reported sterile. Oral prednisolone 0.5 mg/kg was initiated for arthritis. The day after starting the oral prednisolone, he complained of redness, pain, watering and photophobia of the right eye. Vision was 20/120 in the right eye and 20/20 in the left eye. Slit lamp examination showed a slightly superior paracentral shallow corneal ulcer of size 3 × 4 mm with underlying dense stromal infiltrates and significant central stromal haze (Figure 1C). Anterior chamber details were unclear. The left eye was normal on examination.
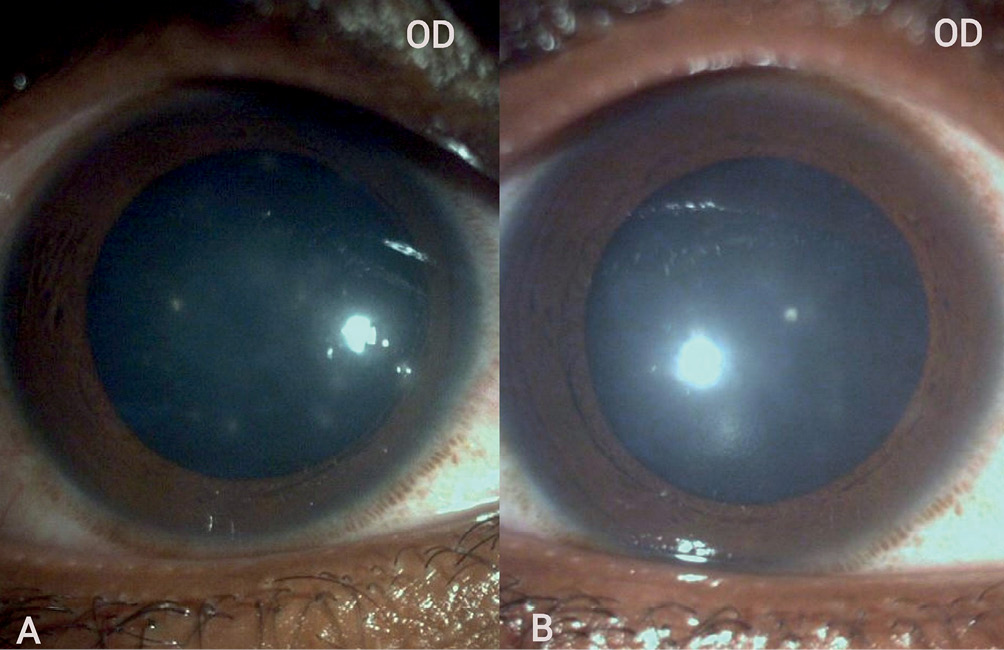
Considering infectious keratitis, corneal scrapings were sent for microbiological evaluation and the patient was started on hourly topical moxifloxacin, lubricants and cycloplegics. Oral prednisolone was discontinued and oral naproxen 250 mg three times a day was initiated for the arthritis. On review after three days, a healing corneal ulcer with persistent stromal infiltrates was noted. With one week of topical antibiotic treatment, the epithelium healed and visual acuity improved to 20/60, but punctate erosions and pleomorphic anterior stromal infiltrates and haze persisted in the right eye (Figure 2A). He also reported minimal symptomatic relief of pain, watering and photophobia. Microbiological evaluation of corneal scrapings was reported as Staphylococcus hominis susceptible to oxacillin, clindamycin, erythromycin and cotrimoxazole. Because of the strong clinical suspicion of the residual keratitis being immune-mediated, topical antibiotic (tobramycin 0.3%) with steroid (loteprednol 0.5%) three times a day and hourly lubricants was started in the right eye. There was dramatic improvement in symptoms and rapid resolution of the stromal infiltrates and haze (Figure 2B) in ten days with topical steroids. Visual acuity improved to 20/20.
Figure 2 Slit lamp photograph showing healed ulcer with pleomorphic anterior stromal infiltrates after one week of topical antibiotics (A). Clear cornea with minimal stromal infiltrates after two weeks of topical steroids (B). OD, right eye oculus dexter
Meanwhile HLA-B27 was reported positive, high-sensitivity C-reactive protein was 49 mg/L, erythrocyte sedimentation rate was 103 mm/hour, and rheumatoid factor and anti-nuclear antibodies were negative. Tuberculin skin test was negative and plain chest radiograph was normal. The patient reported relief of arthritis with oral naproxen and physiotherapy over the next four weeks. At one year follow-up, there were no ocular complaints, arthritis had resolved and there was no inflammatory back pain.
Discussion
The patient fits the diagnosis of ReA in view of age, male gender, preceding infection followed by lower limb predominant arthritis.12 ReA classified under the predominantly peripheral spondyloarthropathy (SpA) family13 has the potential to have sacroilitis and/or spondylitis.2,12 Inflammatory back pain is not rare. The SpA features present in our patient were enthesitis, HLA-B27 positive status and high inflammatory markers.13 Eye disease, namely conjunctivitis, is often seen, among other extra articular manifestations. However, keratitis and corneal ulcer are unusual ocular manifestations of ReA at initial presentation.4-11 We have presented this case because there seemed to be a coexistence of infectious and immune-mediated keratitis in this patient.
The differential diagnosis of a shallow corneal ulcer with underlying stromal infiltrates can either be an early microbial keratitis or an immune-mediated ulcer. Autoimmune diseases and herpetic keratitis are important causes of immune-mediated keratitis.14 Keratitis associated with ReA has been mistaken in the past for herpetic keratitis at initial presentation.11 Among the autoimmune causes, long-standing rheumatoid arthritis followed by systemic lupus erythematosus and granulomatosis with polyangiitis are most frequently associated with immune-mediated keratitis, which is usually peripheral and often associated with anterior scleritis but rarely as early manifestation.15 Our patient did not have a peripheral ulcer.
Lee et al. in a large series identified mild keratitis in only 4 of 113 cases of ReA, although other ocular manifestations were noted in 58% of their patients.4 Kiss et al. reported keratitis in 16 out of 24 patients of chronic ReA at an immunology and uveitis service, but have not discussed the nature or severity of the same.8 First described by Cass in 1949, Mills and Kalina have described the stages of keratitis in their case.5,6 Most of the cases described earlier are mild keratitis, usually subepithelial or stromal, preceded by a prodromal conjunctivitis occurring concurrently or immediately after the onset of joint involvement.4–6,9,11 Our patient also reported conjunctivitis two weeks prior to arthritis.
Keratitis in ReA presenting as a central epithelial defect with an underlying dense, anterior stromal infiltrate has been described earlier in two reports.7,10 Mark et al. reported a case of ReA with bilateral sequential shallow corneal ulcers for which they initiated topical steroids.7 One eye improved, but the other developed a hypopyon, and so steroids were discontinued immediately. Antimicrobial cover appeared to be inadequate, although they did not discuss further management of the case. Lyons et al. reported a patient with an atypical paracentral corneal ulcer with anterior stromal infiltrates mimicking microbial keratitis.10 Our patient seems to closely resemble these cases. Microbiological evaluation revealed S. hominis in our patient, which is a commensal, though it is also known to cause infections.16 Our patient had briefly received oral prednisolone, which may have predisposed him to S. hominis colonisation, but because a true infection could not be ruled, topical antibiotics were added. Despite the antibiotics, he developed stromal keratitis which was concurrent with severe arthritis, thus favouring an immune-mediated pathology. The subsequent resolution of the inflammation on topical steroids also favours this. Lyons reported a similar approach in their case.10 Our case was probably a mixed pathology of super-added infection with inflammation due to ReA. Despite the epithelial healing, he was still symptomatic and had persistent pleomorphic anterior stromal infiltrates. The addition of topical steroids led to his complete recovery in ten days.
Conclusion
Immune-mediated keratitis and corneal ulcer can be an early manifestation of ReA. It is important to perform microbiological evaluation in such cases as super-added infections can occur, and also be watchful that therapy for immune-mediated aetiology is not delayed as it can potentially worsen visual prognosis.
