Telemedicine has come on in leaps and bounds as healthcare systems are streamlined innovatively to meet patient and clinician needs. Healthcare delivery via telemedicine is a viable alternative to face-to-face consultations (FTFC), either in the form of telephone consultations (TC) or video-conferencing (VC) to allow remote communication between clinicians and patients. Additionally, remote monitoring is increasingly available; information such as vital signs or weight is uploaded onto a platform and downloaded by healthcare providers. Healthcare providers utilise telemedicine for remote clinical review and monitoring, and delivering support for self-management of long-term conditions. This is especially vital in the context of the COVID-19 pandemic.
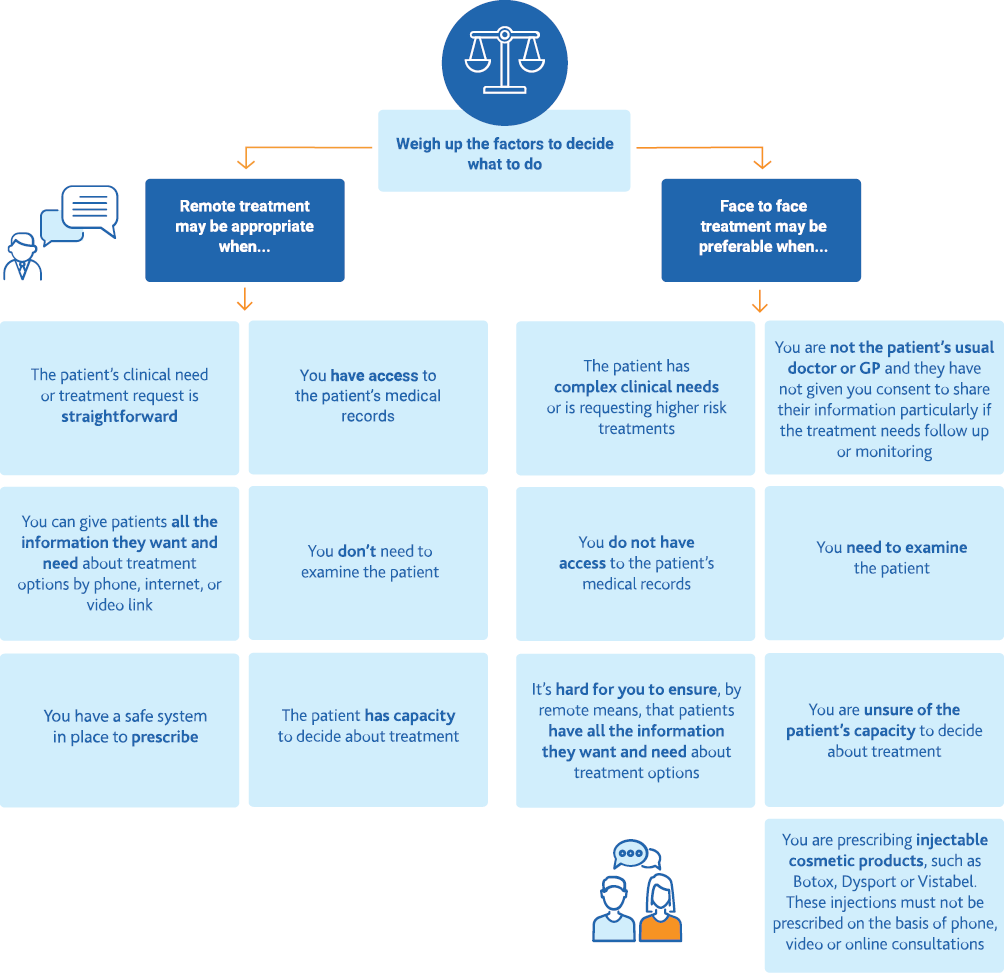
Fundamental to successfully implementing telemedicine is identifying aspects of clinical care and patient groups which may be suitable for this approach. The General Medical Council (GMC) recently published new guidance on how to triage patients safely to TC or FTFC in light of COVID-19 (Figure 1).1 The GMC highlighted two key issues for clinicians – patient consent, which includes their capacity to provide consent, and continuity of care between both parties. The clinical needs of patients, their understanding of their condition and whether physical examination is required are important factors to consider in the decision-making process.
Figure 1 GMC flowchart on factors to determine patient groups suitable for remote or face-to-face consultations1
The Royal College of General Practitioners (RCGP) also published guidelines alongside NHS England and NHS Improvement. This highlighted key principles on safely assessing patients via VC and performing remote physical examinations in general practice. They recommended that a digital ‘total triage’ model could initially be used to determine which patients are most likely suitable for different consultation modalities such as online consultations, TC or VC.2 More importantly, all clinicians should feel comfortable and be competent in the mode of assessment and examination technique before attempting remote examinations. Good information governance policies, informed consent, effective communication skills and safety-netting practices are essential to safely conduct VC and remote examinations.3 Additionally, Greenhalgh published evidence-based guidance on setting up and implementing VC safely in primary care, including situations where VC was deemed appropriate, training on conducting high-quality VC, and assessment of patients with suspected COVID-19.4
How is telemedicine utilised?
Various clinical management pathways in primary or secondary care have adopted virtual technology to assess new patients, monitor chronic conditions or provide education and training; its use covering specialties ranging from cardiovascular disease and diabetes to solid organ transplantation and cancer. A systematic review found telemedicine effective in managing heart failure and improved healthcare outcomes for diabetic patients but less so for other conditions due to the fewer number of studies available.5 Ansary et al demonstrated multiple approaches to incorporating virtual technology into daily clinical practice and provided specific guidelines developed by different specialties.6
Assessment of new patients via telemedicine was considered safe and effective, particularly where geographical barriers exist. This can be useful in secondary care for new patient referrals or follow-up reviews. Duncan et al reported that assessing new neurological referrals via video-link was safe, effective, acceptable by patients and most useful in rural areas.7 Telemedicine safely and effectively replaced 80% of initial visits to a urology clinic from an American male prisoner population.8 Telemedicine was also feasible in managing chronic diseases such as hepatitis C, inflammatory bowel disease (IBD) and diabetes.9–17 For instance, hepatitis C patients who were managed remotely had similar treatment responses to those managed in clinic.9
TC could be an appropriate alternative to FTFC in the community for chronic conditions.18 In a study by Davis et al, type 2 diabetic patients from a rural, underserved community participated in a self-management education programme, ‘Diabetes TeleCare’, which included interactive VC and remote retinal assessment. Conducted by a dietitian and a certified diabetes nurse educator, this showed significant improvements in patients’ glycaemic control and cardiovascular risk.15
Telemedicine for remote monitoring is also increasingly common for chronic conditions. In one study, blood pressure monitoring via mobile health (customised text messages, emails, smartphone apps and wireless blood pressure monitoring) improved blood pressure control through goal-setting.19 Improved glycaemic control was observed in type 1 diabetic patients who received clinical advice based on uploaded information (blood glucose readings, insulin doses, diet and physical activity) on a telemedicine platform.16In another example, patients with rheumatoid arthritis completed questionnaires at pre-determined intervals and if disease remission criteria were not met, a clinical review was triggered.20 Telemedicine platforms for IBD like ‘myIBDcoach’ or ‘Constant-care’ which provide information or self-monitoring tools were associated with improved patient knowledge and reduced outpatient hospital visits, without an increase in relapse or hospital admissions.12,13 All these empower self-management by patients, thus improving treatment adherence.
Do all patients need a physical examination during clinic consultations?
A pertinent issue with the increasing use of telemedicine is the value of physical examination and how clinicians can safely assess patients without physically seeing or touching them.
‘The diagnosis is in the history; examination supports your initial clinical impression.’ Many of us might remember this being mentioned during our formative years of medical school. Does it still ring true? Modern day clinical practice is increasingly reliant on investigations due to the wider availability and higher accuracy of laboratory diagnostics, advanced imaging or endoscopic procedures, not to mention increasingly defensive clinical practice.21,22 Nevertheless, one has to question the importance of physical examination in an outpatient setting. How much value does ‘inspection, palpation, percussion, auscultation’ add to your clinical impression? Does it change how you eventually manage that patient? More importantly, how risky is omitting physical examination once you have elicited their clinical history? Do you already know what investigations or treatment to pursue? Jauhar presents some interesting insights: despite modern medicine devaluing the importance of physical examination due to its perceived inconsistencies and inaccuracies set against a backdrop of rising medical litigation, technology has its flaws and is only as good as its interpreter. Might physical examination come in handy one day to help you clinch the diagnosis when you least expect it?23
There are, of course, more layers to these questions. Clinics with newly referred patients from primary care differ from clinics with follow-up patients. Different approaches are required for individual patients. Certain specialties, for example ophthalmology, otolaryngology and orthopaedics, often require physical examination to formulate differential diagnoses and management plans. Other specialties like gastroenterology, nephrology and endocrinology rely more on investigations largely based on the clinical history. Broadly speaking, many specialty clinics fall somewhere in between; with occasions where a detailed clinical history is often sufficient and others where physical examination is required. Clinicians generally prefer FTFC during the initial visit to establish patient rapport regardless of whether physical examination is necessary.24–26 In primary care, inability to perform examinations were of concern and TC was preferred for follow-up appointments of patients with established diagnoses.25 Similarly, VC was preferred where visual cues were important but physical examination was deemed unnecessary.26 In short, pre-clinic triaging of patients to have TC, VC or FTFC is necessary to ensure clinic appointments are utilised efficiently.
Apart from physical examination, some monitoring usually undertaken during FTFC may be done remotely. In heart failure patients, remote structured interventions i.e. daily weights, blood pressure measurements and ECG recordings were successfully undertaken, and were associated with a decreased percentage of days lost due to unplanned cardiovascular hospital admissions and all-cause mortality.27
Can a physical examination be done remotely and effectively?
There are nuances to telemedicine consultations. Non-verbal cues (facial expressions, body language, severity of illness and patient frailty) have always been crucial in building a good doctor-patient relationship. During TC, both parties are deprived of this and therefore need to rely on advanced verbal skills to avoid making judgment errors. Clinicians and patients have expressed concerns about making inaccurate diagnoses with TC but agreed that an existing doctor-patient relationship would alleviate this.25 As a solution, some have adapted specific questioning methods and instructions for patients to self-examine to elicit important clinical information. This is, however, not always appropriate.28
VC provides a platform for remote face-to-face contact, allowing the use of non-verbal cues and physical examination, either with an assistant beside the patient or aided by sophisticated devices such as video otoscopes, electronic stethoscopes and dermatoscopes. Here are some examples of how physical examination has been adapted in VC. Tanaka et al developed a virtual orthopaedic examination protocol using a pre-appointment checklist for patients and specific instructions on camera-positioning, body-positioning, setting and attire to maximise consultation efficiency.29Buvik et al evaluated video-assisted orthopaedic consultations where a trained nurse assisted the patient with physical examination and found non-inferiority of VC to standard consultations.30In neurosurgery, VC with a medical assistant beside the patient was associated with positive experiences by clinicians and patients, albeit with limitations to the examination – assessment of tone, strength between limbs, visual fields and reflexes.31
Dermatology, a specialty that relies heavily on physical examination, has evolved rapidly by taking advantage of high-resolution smartphone cameras and apps to aid remote assessment. Lesion assessments via artificial intelligence developed through deep convolutional neural networks were comparable to experts in one study and outperformed specialists in another.32,33 This innovative technology has even extended to retinal assessment, whereby a meta-analysis concluded high diagnostic accuracy of digital imaging in diabetic retinopathy.34
Nevertheless, there are some considerations. Pappas et al reported that in a vascular clinic where specialists relied on primary care nurses to report physical findings, both patients and clinicians felt a sense of loss of control in the consultation.35 Another study in the Emergency Department on the assessment of sore throat reported poor concordance of a VC physical examination with FTFC.36 In situations where technological deficiencies do not permit its usage or in specific scenarios where a chest or abdominal examination is needed, FTFC remains the default option. In the current climate, newly referred patients or select follow-up patients can be reviewed via FTFC with appropriate personal protective equipment (PPE) use if physical examination is deemed necessary by the clinician or in fact, to establish a solid doctor-patient relationship. Overall, VC overcomes many obstacles in remote consultations with the caveat that appropriate technology and setup are available; in other settings where these do not apply, FTFC with adequate PPE is still required.
How do patients feel about telemedicine?
Until recently, telemedicine has been optional, particularly between tertiary centres and rural populations. COVID-19 has forced many services to restructure outpatient pathways and consider incorporating telemedicine to minimise face-to-face contact. When implemented appropriately, there is no doubt telemedicine has its advantages and this ‘mini revolution’ could turn out to be a silver lining.
Telemedicine removes the need for patients to rearrange commitments, travel long distances for 10-minute appointments or endure prolonged waits in hospital for specialist reviews, particularly for follow-up of chronic diseases. This saves time and travel costs with less disruption to patients’ daily routines and better access to appointments. Multiple studies across various specialties have reported that telemedicine is well-received with high satisfaction rates, particularly by patients with significant mobility issues, busy childcare or work responsibilities, those living in rural areas or elderly patients with multiple comorbidities.13,31,37–40 One review found VC to be acceptable and comfortable for patients treated for human immunodeficiency virus (HIV).37Improved flexibility for both clinicians and patients leads to improved patient attendance and compliance. It would be interesting to explore whether this reduces the rate of non-attendances which will maximise clinic efficiency and hence reduce waiting times for first-appointment specialist referrals.
Correct identification of suitable patients for telemedicine is key to ensuring safe clinical care and patient satisfaction.41 They could be identified by a pre-clinic questionnaire or clinician triage. An unchanged clinical condition in a previously stable patient or where no new issues were highlighted suggests these patients could be triaged into virtual clinics rather than FTFC.41 A vital aspect worth noting is that telemedicine is most effective when there is an established doctor-patient relationship with mutual trust, or for long-term conditions where physical examination is unnecessary.42,43 In one study, stable patients on peritoneal dialysis who were reviewed via VC had significantly fewer hospital admissions.44
Telemedicine has an overall positive impact on patients’ and clinicians’ satisfaction.38 However, drawbacks include issues with technology, governance issues and difficulty performing physical examinations.24,39,40 Implementing telemedicine will require reconfiguration of technological systems and clinical and administrative pathways to allow its seamless integration into routine clinical practice.45 Sufficient training to enable staff to troubleshoot issues that may arise is crucial. Ensuring safety of patient data is paramount and needs to be carefully considered in the setup and maintenance of telemedicine. Besides ensuring that appropriate devices are available for them, we need patients to willingly prefer and engage with TC or VC over FTFC for telemedicine to be sustainable in the long term.
As demonstrated above, multiple studies conducted in the past few years pre-COVID-19 have shown a willingness by healthcare providers to innovate by introducing virtual consultation and examination into daily clinical practice. Despite this, the majority of consultations were still conducted via FTFC. It is undeniable that the pandemic and post-COVID-19 landscape has exponentially accelerated the implementation of these changes. Whilst the current default practice in many healthcare establishments is for TC, patients could be offered a FTFC based on clinician triage, if they have sensory or cognitive impairment, if they have learning disabilities or if they lack appropriate technological devices and setups for telemedicine. This would prevent them from becoming disadvantaged by the sweeping changes post pandemic.
Conclusion
Telemedicine is not a ‘one-size-fits-all’ alternative to conventional models of delivering outpatient clinical care. It appears to be an alternative in outpatients when applied to specific patient cohorts. The majority of evidence suggests that stable patients with chronic disease who have a previously established relationship with their specialists are most suitable for telemedicine.
As for the feasibility and safety of virtual physical examinations, there is some variability. Some specialties have demonstrated ways of adapting it via advanced technology or the assistance of another healthcare worker, with very few reported adverse events. Evidence of serious misdiagnoses or mismanagement of patients due to virtually adapted examinations is lacking and requires further research.
Healthcare providers have been forced by the pandemic to adapt rapidly to deliver safe and good quality care. Perhaps clinicians will be prompted to rethink the importance of physical examination and its value in patient assessment. Moving forward, telemedicine will be increasingly adopted. However, it will be important to gauge its impact on healthcare systems and pathways as clinical care provision evolves in the aftermath of the COVID-19 pandemic.46
References
1 General Medical Council. Remote consultations: is a remote consultation appropriate? [Internet]. GMC: 2020 [Accessed 10 September 2020]. Available from: https://www.gmc-uk.org/ethical-guidance/ethical-hub/remote-consultations
2 NHS England and NHS Improvement. Advice on how to establish a remote ‘total triage’ model in general practice using online consultations. [Internet]. Covid-19 Ad hoc guidelines: 2020 [Accessed 20 September 2020]. Available from: https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/...
3 NHS England and NHS Improvement. Principles of safe video consulting in general practice during COVID-19 [Internet]. 29 May 2020 [Accessed 1 September 2020]. Available from: https://www.networks.nhs.uk/nhs-networks/releasing-capacity-in-general-p...
4 Greenhalgh T. Video consultations: a guide for practice [Internet]. BJBP 18 March 2020 [Accessed 1 September 2020]. Available from: https://bjgplife.com/2020/03/18/video-consultations-guide-for-practice
5 Flodgren G, Rachas A, Farmer AJ et al. Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2015; 557.
6 Ansary AM, Martinez JN, Scott JD. The virtual physical exam in the 21st century. J Telemed Telecare 2019.
7 Duncan C, Dorrian C, Crowley P et al. Safety and effectiveness of telemedicine for neurology outpatients. Scott Med J 2010; 55: 3-5.
8 Sherwood BG, Han Y, Nepple KG et al. Evaluating the effectiveness, efficiency and safety of telemedicine for urological care in the male prisoner population. Urol Pract 2018; 5: 44-51.
9 Arora S, Kalishman S, Thornton K et al. Expanding access to hepatitis C virus treatment--Extension for Community Healthcare Outcomes (ECHO) project: disruptive innovation in specialty care. Hepatology 2010; 52: 1124-33.
10 Rossaro L, Torruellas C, Dhaliwal S et al. Clinical outcomes of hepatitis C treated with pegylated interferon and ribavirin via telemedicine consultation in Northern California. Dig Dis Sci 2013; 58: 3620-25.
11 Pedersen N, Elkjaer M, Duricova D et al. eHealth: Individualisation of infliximab treatment and disease course via a self-managed web-based solution in Crohn’s disease. Aliment Pharmacol Ther 2012; 36: 840-49.
12 Elkjaer M, Shuhaibar M, Burisch J et al. E-health empowers patients with ulcerative colitis: a randomised controlled trial of the web-guided ‘Constant-care’ approach. Gut 2010; 59: 1652-61.
13 de Jong MJ, van der Meulen-de Jong AE, Romberg-Camps MJ et al. Telemedicine for management of inflammatory bowel disease (myIBDcoach): a pragmatic, multicentre, randomised controlled trial. Lancet 2017; 390: 959–68.
14 Liu W, Saxon DR, McNair B et al. Endocrinology telehealth consultation improved glycemic control similar to face-to-face visits in veterans. J Diabetes Sci Technol 2016; 10: 1079-86.
15 Davis RM, Hitch AD, Salaam MM et al. TeleHealth improves diabetes self-management in an underserved community: diabetes TeleCare. Diabetes Care 2010; 33: 1712-17.
16 Ruiz de Adana MS, Alhambra-Expósito MR, Muñoz-Garach A et al. Randomized study to evaluate the impact of telemedicine care in patients with type 1 diabetes with multiple doses of insulin and suboptimal HbA(1c) in Andalusia (Spain): PLATEDIAN Study. Diabetes Care 2020; 43: 337-42.
17 Siegel CA. Transforming gastroenterology care with telemedicine. Gastroenterology 2017; 152: 958-63.
18 Downes MJ, Mervin MC, Byrnes JM et al. Telephone consultations for general practice: a systematic review. Syst Rev 2017; 6: 128.
19 Li R, Liang N, Bu F et al. The effectiveness of self-management of hypertension in adults using mobile health: systematic review and meta-analysis. JMIR mHealth uHealth 2020; 8: e17776.
20 Piga M, Cangemi I, Mathieu A et al. Telemedicine for patients with rheumatic diseases: Systematic review and proposal for research agenda. Semin Arthritis Rheum 2017;47:121-28.
21 Jaques H. Number of doctors facing medicolegal claims increases by 15%. BMJ 2013; 347.
22 Price P. Current and future challenges facing medico-legal experts – An expert’s view. J Patient Saf Risk Manag 2018; 23: 109–13.
23 Jauhar S. The demise of the physical exam. N Engl J Med 2006; 354: 548-51.
24 Hiratsuka V, Delafield R, Starks H et al. Patient and provider perspectives on using telemedicine for chronic disease management among Native Hawaiian and Alaska Native people. Int J Circumpolar Health 2013; 72.
25 McKinstry B, Watson P, Pinnock H et al. Telephone consulting in primary care: a triangulated qualitative study of patients and providers. Br J Gen Pract 2009; 59: e209-18.
26 Hammersley V, Donaghy E, Parker R et al. Comparing the content and quality of video, telephone, and face-to-face consultations: a non-randomised, quasi-experimental, exploratory study in UK primary care. Br J Gen Pract 2019; 69: e595-e604.
27 Koehler F, Koehler K, Deckwart O et al. Efficacy of telemedical interventional management in patients with heart failure (TIM-HF2): a randomised, controlled, parallel-group, unmasked trial. Lancet 2018; 392: 1047-57.
28 Lopriore S, LeCouteur A, Ekberg K et al. ‘You’ll have to be my eyes and ears’: A conversation analytic study of physical examination on a health helpline. J Clin Nurs 2019; 28: 330-39.
29 Tanaka MJ, Oh LS, Martin SD et al. Telemedicine in the era of COVID-19: The virtual orthopaedic examination. J Bone Joint Surg Am 2020; 102: e57.
30 Buvik A, Bugge E, Knutsen G et al. Quality of care for remote orthopaedic consultations using telemedicine: a randomised controlled trial. BMC Health Serv Res 2016; 16: 483.
31 Blue R, Yang AI, Zhou C et al. Telemedicine in the era of COVID-19: a neurosurgical perspective. World Neurosurg 2020; 139: 549-57.
32 Esteva A, Kuprel B, Novoa RA et al. Dermatologist-level classification of skin cancer with deep neural networks. Nature 2017; 542: 115-18.
33 Haenssle HA, Fink C, Schneiderbauer R et al. Man against machine: diagnostic performance of a deep learning convolutional neural network for dermoscopic melanoma recognition in comparison to 58 dermatologists. Ann Oncol 2018; 29: 1836-42.
34 Shi L, Wu H, Dong J et al. Telemedicine for detecting diabetic retinopathy: a systematic review and meta-analysis. Br J Ophthalmol 2015; 99: 823-31.
35 Pappas Y, Seale C. The physical examination in telecardiology and televascular consultations: a study using conversation analysis. Patient Educ Couns 2010; 81: 113-18.
36 Akhtar M, Van Heukelom PG, Ahmed A et al. Telemedicine physical examination utilizing a consumer device demonstrates poor concordance with in-person physical examination in emergency department patients with sore throat: a prospective blinded study. Telemed J E Health 2018; 24:790-96.
37 León A, Cáceres C, Fernández E et al. A new multidisciplinary home care telemedicine system to monitor stable chronic human immunodeficiency virus-infected patients: A randomized study. PLoS One 2011; 6: e14515.
38 Orlando JF, Beard M, Kumar S. Systematic review of patient and caregivers’ satisfaction with telehealth videoconferencing as a mode of service delivery in managing patients’ health. PLoS One 2019; 14: e0221848.
39 Sabesan S, Simcox K, Marr I. Medical oncology clinics through videoconferencing: an acceptable telehealth model for rural patients and health workers. Intern Med J 2012; 42: 780-85.
40 Gordon HS, Solanki P, Bokhour BG et al. ‘I’m Not Feeling Like I’m Part of the Conversation’ Patients’ perspectives on communicating in clinical video telehealth visits. J Gen Intern Med 2020; 35: 1751-58.
41 Hunter J, Claridge A, James S et al. Improving outpatient services: the Southampton IBD virtual clinic. Postgrad Med J 2012; 88: 487-91.
42 Shaw SE, Seuren LM, Wherton J et al. Video consultations between patients and clinicians in diabetes, cancer, and heart failure services: linguistic ethnographic study of video-mediated interaction. J Med Internet Res 2020; 22: e18378.
43 Jordan DN, Jessen CM, Ferucci ED. Views of Patients and Providers on the Use of Telemedicine for Chronic Disease Specialty Care in the Alaska Native Population. Telemed J E Health 2021; 27: 82-89.
44 Gallar P, Vigil A, Rodriguez I et al. Two-year experience with telemedicine in the follow-up of patients in home peritoneal dialysis. J Telemed Telecare 2007; 13: 288-92.
45 Wherton J, Shaw S, Papoutsi C et al. Guidance on the introduction and use of video consultations during COVID-19: important lessons from qualitative research. BMJ Leader 2020; 4: 120-23.
46 Romanick-Schmiedl S, Raghu G. Telemedicine — maintaining quality during times of transition. Nat Rev Dis Primers 2020; 6: 45.