Introduction
Sinusitis describes inflammation or swelling of the sinuses and most commonly results from infection. The typical symptoms of acute sinusitis are nasal congestion, nasal discharge, facial pain or pressure, and reduction in smell, lasting less than four weeks with a sudden onset of symptoms.1 Acute sinusitis is one of the most common infectious diseases seen in general practice; its incidence is 15–40 episodes per 1,000 patients per year.2 The vast majority of cases are viral in origin, with an estimate of approximately 2% of cases presenting to GPs being caused by a bacterial infection.3
Acquired oculomotor nerve palsies are rare (4.0 per 100,000) and the most common causes are microvascular, trauma, neoplasm, post-surgical complication and aneurysm.4 An oculomotor (third cranial nerve) palsy is an important clinical sign as, although rare, it can indicate the presence of a life-threatening aneurysm or other serious pathology.
This case of acute sinusitis causing isolated oculomotor nerve palsy is presented because of its unusual nature, to educate medical professionals of a rare complication of a common disease and to improve differential diagnosis of cranial nerve palsy.
Case presentation
A fit and well 64-year-old male presented to his GP with a one-week history of nasal congestion and frontal sinus pain, together with a one-day history of a drooping left eyelid (ptosis). The patient re-presented the following day with worsening ptosis and a dilated pupil. At both presentations, the appearance of the skin around the orbit was normal. There was no history of weight loss and no atherosclerotic risk factors. There was no relevant family history. The patient reported being a non-smoker and to be generally fit and active. Examination detected left ptosis with left mydriasis. There was no papilloedema, and the rest of the cranial nerve and peripheral nervous system examination was normal. There was no palpable thyroid gland or cervical lymph nodes. He was diagnosed with a partial oculomotor (third cranial nerve) palsy and referred to the Emergency Department. The acute medical team confirmed the neurological examination, and he was referred to the Neurology service.
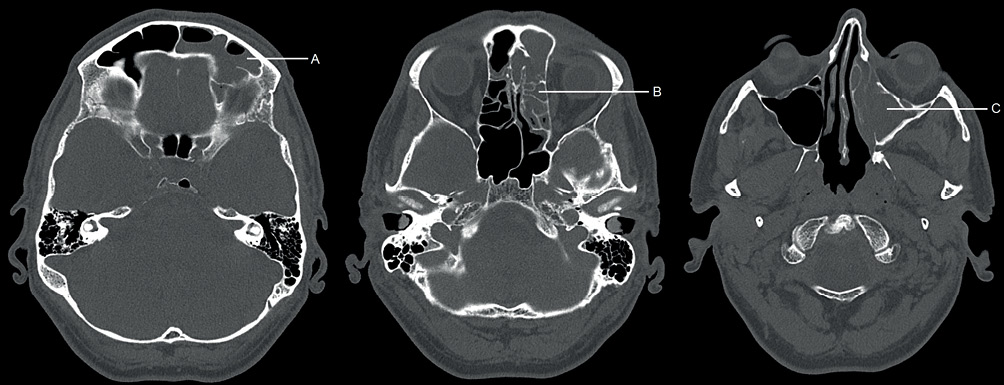
Non-contrasted computed tomography (CT) of the head (Figure 1) together with intravenous contrasted CT angiography of the intracranial vessels demonstrated no acute intracranial haemorrhage, subdural collection, major territory infarct or mass lesion with patent intracranial arteries, and no identifiable intracranial aneurysm or vascular malformation. Positive findings included mucosal thickening in the left frontal sinus, left ethmoid air cells and left maxillary sinus. There was also minor mucosal thickening in the right maxillary sinus and ethmoid air cells. The significant mucosal thickening of the sinuses on the left side raised the possibility of obstruction of the left ostiomeatal complex. Taken together, these findings supported a clinical diagnosis of a sinus infection.
Figure 1 Non-contrasted axial bone window CT imaging of the head showing widespread mucosal thickening of the paranasal sinuses. A: mucosal thickening in the left frontal sinus; B: mucosal thickening in the left ethmoid air cells; C: mucosal thickening in the left maxillary sinus
Full blood count showed elevated white cell count (12.4 × 109/L, normal range 4.0–11.0 × 109/L), neutrophils (9.3 × 109/L, normal range 2.0–7.5 × 109/L) and monocytes (1.2 × 109/L, normal range 0.2–0.8 × 109/L). Serum biochemistry tests showed C-reactive protein was also elevated (66 mg/L, normal <10 mg/L). No other abnormalities were identified on serum testing.
Cerebrospinal fluid (CSF) microscopy and culture revealed an acellular sample, with no organism growth in primary culture or enrichment broth. CSF protein was slightly elevated at 0.62 g/L (normal range 0.15–0.45 g/L), with unremarkable CSF glucose (3.7 mmol/L, normal range 2.8–5.0 mmol/L) and plasma glucose (5.3 mmol/L, normal range <11.1 mmol/L).
Acquired oculomotor nerve palsy is most commonly caused by microvascular disturbance (diabetes, high blood pressure), trauma (including recent neurosurgery), neoplasm and aneurysm.4 This patient was not diabetic and blood pressure was within the normal range for his age, sex and ethnicity (129/91 mmHg). The patient reported no recent history of trauma or neurosurgery. Cranial CT imaging showed no evidence of neoplasm or aneurysm.
There was symptomatic, radiographic and biochemical evidence to support the clinical suspicion of sinusitis on the affected side of the oculomotor palsy. As oculomotor nerve palsy has rarely been associated with sinusitis,5 and in the absence of any other proven aetiology, the patient was diagnosed with oculomotor palsy secondary to sinusitis.
The patient was prescribed intranasal steroids for five weeks, xylomethazoline three times a day for ten days and nasal douching. The patient reported that all symptoms, including ptosis, resolved within one week of treatment. A neurology follow-up three months later revealed no recurrence
of symptoms.
Discussion
Acute sinusitis is a common disease, and typical symptoms include nasal congestion, nasal discharge, facial pain or pressure and reduction in smell, lasting less than four weeks and with a sudden onset of symptoms. Isolated cranial nerve palsies are most commonly caused by microvascular dysfunction, trauma, neoplasm, post-surgical complication and aneurysm.4 In this case, we believe sinusitis was the underlying cause of the oculomotor nerve palsy observed due to mucosal thickening of the sinuses, resulting in obstruction of the ostiomeatal complex. The levator palpebrae superioris muscle is responsible for elevation of the eyelid and is innervated by the superior division of the oculomotor nerve. The third cranial nerve emerges from the anterior end of the cavernous sinus, and then passes along the upper part of the lateral wall of the sphenoidal and posterior ethmoidal sinuses.6 It is likely that direct compression of the nerve at this point within the ethmoid sinus, secondary to the sinusitis, resulted in the observed ptosis. The CT scan demonstrates clear involvement of the ethmoidal sinus on the symptomatic side. This explanation is also supported by the localised nature of the patient’s symptoms, and the resolution of the symptoms with treatment of the sinusitis. It is unlikely that the symptoms were a result of the involvement of the cavernous sinus, as the clinical evidence presented does not fit with this concept. There is no strong evidence from this case to suggest orbital involvement; there was no papilloedema and no involvement of other cranial nerves, and the appearance of the skin around the orbit was normal.
There are limited case studies reporting cranial nerve palsy as an unusual complication of sinusitis, including oculomotor nerve palsy as a result of sphenoid sinusitis,7 Raeder syndrome (paratrigeminal oculosympathetic syndrome) associated with bacterial sinusitis,8 abducens nerve palsy as a complication of sphenoid sinusitis9–11 and isolated ptosis as a complication of sinusitis.12 A review identified 17 patients with cranial nerve palsy as a result of sinusitis, and indicated that the abducens nerve was the cranial nerve most frequently affected (76%), followed by the oculomotor nerve (18%). The review identified purulent sphenoid sinusitis as the most common underlying cause (64% of cases), followed by allergic fungal sinusitis in 18% of cases.5
Conclusion
This case report adds to the limited literature reporting oculomotor nerve palsy, in particular isolated ptosis, resulting from sinusitis. We wish to raise awareness of this unusual complication and to add to the case literature demonstrating cranial nerve palsy as a complication of sinusitis so that differential diagnosis of cranial nerve palsy may be improved in the future.
