A 74-year-old male presented to hospital with a febrile illness and right-sided abdominal discomfort. He had visited his GP in the preceding two weeks with dysuria, increased urinary frequency, right-sided loin pain and fever. Despite two courses of oral antibiotics for a presumed urinary tract infection, his symptoms failed to resolve completely.
His past medical history includes an elective laparoscopic cholecystectomy approximately one year ago for symptomatic gallstone disease. This was complicated by a bile leak, which was treated with biliary stenting via endoscopic retrograde cholangiopancreatography and a brief stay in an intensive care unit. He subsequently made a full recovery and has been well until the most recent admission. He also has autoimmune hepatitis with cirrhosis, which is controlled on a stable dose of Azathioprine 75 mg OD and Prednisolone 7.5 mg OD.
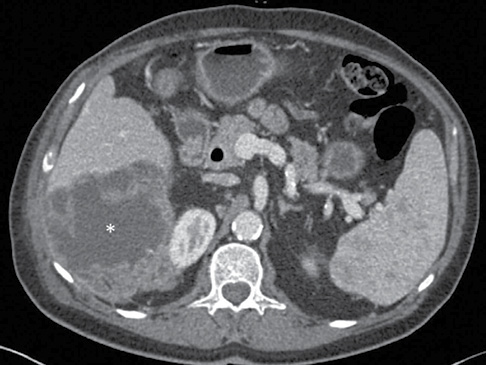
Initial blood tests showed raised inflammatory markers with white cell count of 14 × 109/L (normal range 4.5–11 × 109/L), C-reactive protein of 71 mg/L (normal range 0–10 mg/L) and mildly cholestatic liver function tests with a normal bilirubin. A contrast-enhanced computed tomography (CT) scan of his abdomen (Figure 1) was obtained which reported a large cystic lesion, approximately 11 cm in diameter, from the right lobe of the liver with extension to abut the right kidney, with associated right peri-renal and splenic inflammatory change. This was not evident on a CT from two years ago or on a liver ultrasound scan four months previously. The most likely diagnosis was thought to be a hepatic abscess.
Figure 1 Axial view of post-contrast CT abdomen showing 11 cm liver abscess (see asterisk).
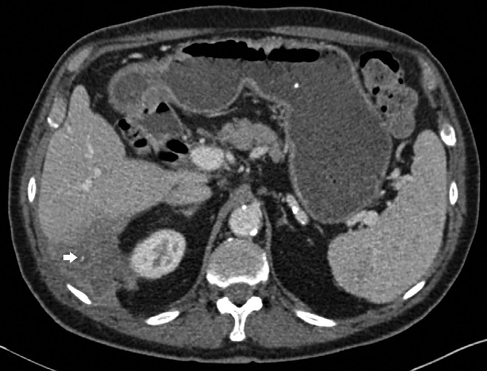
He was treated with IV co-amoxiclav 1.2 g TDS and ultrasound guided percutaneous drainage of the abscess. Culture of the aspirate was positive for Proteus mirabilis and Escherichia coli. An interval CT scan ten days post-drainage confirmed a reduction in the size of the collection (Figure 2). Following microbiological advice, treatment was changed to once-daily IV ertepenem 1 g OD on an outpatient basis.
We discussed the patient’s case with a hepato-pancreato-biliary radiologist to determine the exact origin of the abscess and further assess the peri-nephric changes in order to guide future management of the patient beyond the immediate care of antibiotics and drainage. It was concluded that this collection represented a peri-hepatic abscess with a small hyperdense spot seen in the posterior aspect of the collection (arrow, Figure 2). This most likely represents a dropped gallstone in Morison’s pouch from previous cholecystectomy and the peri-nephric changes were likely to be reactive.
Figure 2 Axial view of post-contrast CT abdomen following 21 days of IV antibiotics and 10 days of percutaneous drainage (drain now removed). Partial resolution of abscess seen.
A dropped stone is a recognised complication of laparoscopic cholecystectomy with an estimated incidence of 5–40%.1 However, the development of a septic complication is rare, and a conservative approach is often recommended in incidentally discovered cases. In patients with a septic complication, further intervention is required.1 In this patient, this became a nidus for abscess and, for a patient on immunosuppression, it is likely to be a recurring problem. We therefore referred the patient for surgical exploration and removal of the stone.
There are a few points worth highlighting about the management of this patient. First, cholecystectomy is one of the commonest elective surgical procedures performed worldwide. Although recovery is generally uncomplicated, clinicians need to be aware of specific complications that are associated with potentially significant morbidity, such as the sequelae of a dropped stone.2 This may not become evident for years following surgery and may manifest as a localised septic process or phenomena such as fistulation through the diaphragm.3 Surgical exploration to retrieve such stones is fraught with difficulty due to the re-operative field and challenges from a ‘needle in a haystack’ situation. Early involvement of a specialist interventional radiologist through a collaborative approach with a specialist medical gastroenterologist is therefore the favoured approach to these cases.
Second, given the ever-increasing use of cross-sectional imaging in day-to-day management of patients, radiologists are constantly under pressure to report scans on time, often with limited information available to them. It is therefore the responsibility of the treating physician to discuss any case where the report does not fully correlate with the clinical picture.
In summary, awareness of long-term complications and approaching these cases through a multi-disciplinary combined approach (gastroenterologist/interventional radiologist/hepatobiliary surgeon) will give the highest chance of successful outcome and should be widely encouraged.
