In an era where time is a scarce commodity and technology seems to dominate clinical medicine, we are in danger of neglecting the value of the physical examination (PE). The COVID-19 pandemic has further challenged our place at the bedside and the way we both practice and teach the PE. Personal protective equipment (PPE) can dull the senses by altering sight, smell and touch. Gloves make assessment of the radial pulse difficult. Disposable stethoscopes or the background noise from a powered respirator compromise auscultation, and the face-to-face contact required for ophthalmoscopy inhibits its use.
But, despite these difficulties, PE has contributed to the care of COVID patients,1 teaching has continued2 and COVID-19 will not be the death knell for the PE. We describe seven reasons why the PE remains important, updating a framework of utility that our group has described elsewhere.3
1. PE contributes to diagnosis
In the largest published study,4 set in an emergency room setting, the single modality contributing most to diagnosis was the history. Some 61% of diagnoses were made by history and examination, without recourse to laboratory tests or imaging. Clinical context determines the relative utility of history, examination, imaging and laboratory tests, and, in general, as diagnostic classification becomes more refined, clinical information becomes proportionately less important. However, at first presentation in community or hospital practice, core clinical information remains central to primary diagnosis and the appropriate selection of subsequent supporting diagnostic tests.
2. Prognosis and ongoing care
In routine generalist practice, efficacy of treatment is commonly judged on the basis of clinical findings, for example, symptoms and signs of fluid retention and elevated filling pressures in a heart failure patient. We may add a chest radiograph, brain-natriuretic peptide, or echocardiogram, but in most settings, for most patients and most doctors, physical assessment remains fundamental. Furthermore, simple clinical findings, such as an elevated JVP or third heart sound, have independent prognostic value in patients with heart failure.5 In COVID-19 infection, respiratory rate on admission is a significant predictor of outcome.6
3. Patient safety
If you don’t do the physical examination, you will make mistakes.
Just as the presence of PE makes a positive contribution to clinical care, its absence compromises patient safety.
A patient history is described in text box 1. The absence of PE, in this simple case, caused distress to the patient, concern to his family, and exposed the patient to the multiple dangers and costs of an unnecessary hospital admission.
Box 1 A case of delayed diagnosis due to inadequate PE
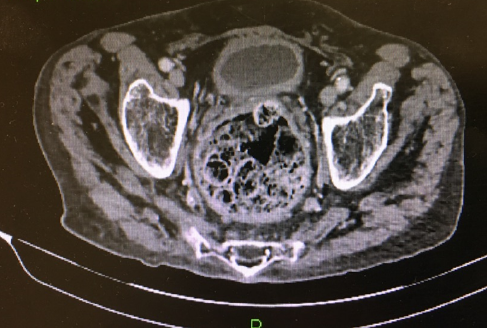
An 82-year-old care home resident became agitated and aggressive to his carers. He had dementia but no other major comorbidity. Judged unmanageable in the care home he was sent to an acute receiving unit with a provisional diagnosis of delirium likely due to infection. Basic bloods were normal, but he was started on antibiotics and admitted to hospital where he was noted to be incontinent of liquid faeces. A CT of the abdomen was requested (Figure 1). It showed a large ball of inspissated faeces in the rectum and extensive colonic faecal impaction. Subsequently, simple palpation of the abdomen and digital rectal examination (DRE) confirmed the CT findings. Prior documentation of the PE in his case file noted ‘Abdo NAD’ and there was no record, in hospital or in the care home, of a prior DRE. After disimpaction, all aggressive behaviour resolved.
Figure 1 CT of pelvis and rectum showing faecal impaction
A major report highlighted the significance of diagnostic error in the USA, estimating that 18 million diagnostic errors occur per year, and that almost all patients are exposed to diagnostic error at some time in their life.7
The report also indicated that flaws in basic clinical information contributed to diagnostic error, a point emphasised by a study detailing almost 300 patient vignettes in which problems with the PE contributed to error. In this study, the dominant clinician error was not the misinterpretation of PE findings, but simply that, in some 60% of patients, there was no record that the PE had actually been performed.8
4. Patient contact
The physical examination takes you to the bedside – that’s where the patient is.
More than 50% of US trainee time is spent administering to the representation of the patient on a computer screen (the ‘i-Patient’) rather than the patient themselves.9 Patients find value in the PE,10 and expect their physicians to perform one. A well-performed PE can have a placebo effect,11 but, done poorly, or not at all, can be detrimental to the patient-physician relationship. Physicians also find meaning and professional fulfilment through contact with patients.12 The current epidemic of stress and burnout is in part due to lack of time spent with patients.13
5. Teaching observation
“The whole art of medicine is in observation.”
Sir William Osler
James Parkinson described his eponymous disease almost exclusively on the basis of observation – cogwheel rigidity one of the very few signs he did not describe.14 Observation has even greater importance during the pandemic, as practiced through a telemedicine consultation, a hospital room doorway, or even a car window at a drive-through COVID-19 testing station. Although observation is best taught in the presence of the patient, numerous studies have shown that teaching intentional observation in other contexts (e.g. taking medical students to an art gallery to describe a painting) improves the ability to recognise PE findings.15 Much can be gleaned from facial expressions, clothing, stature, habitus, positioning and gait,16 that cannot be derived from the electronic health record. In the pandemic, the ability to recognise asymmetric chest wall expansion may aid the diagnosis of pneumonia, pleural effusion or pneumothorax.17
6. Teaching clinical reasoning
Teaching physical examination takes you to the bedside – that’s where the patient is.
Diagnosis is dependent upon the gathering and synthesis of relevant information, with the ability to gather information as important as the ability to synthesise. Information gathering skills can be taught at the bedside in a hypothesis-driven fashion which encourages the learner to choose and interpret relevant PE manoeuvres.18,19 Simulation supports the acquisition of clinical skills, but should be seen as complementary, and not a standalone alternative. Learning PE in the presence of the patient teaches many other skills, such as communication, rapport-building, professionalism, and perhaps most importantly, how to navigate uncertainty.19
7. Reducing over-investigation
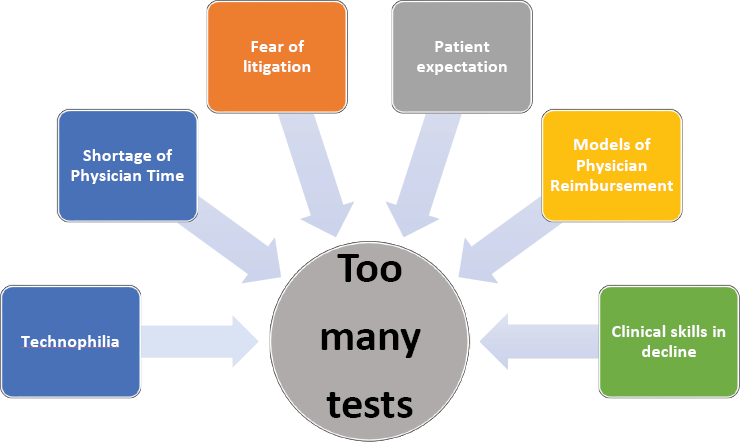
Few disagree that over-testing is endemic in Western medicine. Our own synthesis of the likely reasons for this is shown in Figure 2. A ‘vicious cycle’ now exists in which PE is practiced less, consequently taught less, and consequently assessed less – which leads back to it being practised less. While we do not yet have hard data, we suggest that more frequent use of a hypothesis-driven PE would help break this cycle, increase diagnostic accuracy, improve patient-physician relationships, reduce unnecessary testing, and decrease the overall cost of care.
Figure 2 Some reasons for over-testing
Conclusion
The COVID-19 pandemic has challenged bedside medicine in many ways. Clinical practice, teaching, and assessment have all been compromised. But we have already adapted our practice and will evolve that practice further.
The PE has a strong evidence base,17 but, like all investigations, has limitations. There is however a difference between something of limited value and something of no value. Current exhortations that the stethoscope is worthless and can be discarded are dangerous and simply risk reducing confidence of both patients and doctors in the tools most frequently available to them.
New curricula for teaching PE should be developed and focus on manoeuvres or signs with best supporting evidence of value, derived from specific studies of utility,17 or surveys of what clinicians actually find useful in practice.20
Bedside diagnostic technology will continue to develop. We strongly support the teaching and practice of point-of-care ultrasound (POCUS),20 but recognise its limitations too. Furthermore, the barriers to competent practice of POCUS are broadly similar to those said to inhibit PE.
The acquisition of all bedside skills requires deliberate practice, directly observed by trainers who provide immediate feedback, and clear standards of competence against which to assess learners. Physical examination, like POCUS, needs to be taught, assessed and practised if it is to be of maximum value. It is complementary to, and not in competition with, technology. Our challenge is to find the time and create the learning environment to cultivate these valuable skills for those who will follow us.
References
1 Garibaldi BT, Chisolm MS, Berkenblit GV et al. Review of the published literature to characterise clinical excellence in COVID-19 care. Postgrad Med J 2021.
2 Russell SW, Ahuja N, Patel A et al. Peabody’s paradox: balancing patient care and medical education in a pandemic. J Grad Med Educ 2020; 12: 264-68.
3 Zaman J, Verghese A, Elder A. The value of physical examination: a new conceptual framework. South Med J 2016;109: 754-57.
4 Paley L, Zornitzki T, Cohen J et al. Utility of clinical examination in the diagnosis of emergency department patients admitted to the department of medicine of an academic hospital. Arch Intern Med 2011; 171: 1394-96.
5 Elder A, Japp A, Verghese A. How valuable is physical examination of the cardiovascular system? BMJ 2016; 354: i3309.
6 Garibaldi BT, Fiksel J, Muschelli J et al. Patient trajectories among persons hospitalized for COVID-19: a cohort study. Ann Intern Med 2021; 174: 33-41.
7 Balogh EP, Miller BT, Ball J (editors). Improving diagnosis in health care. National Academies of Sciences, Engineering, and Medicine. Washington, DC: The National Academies Press; 2015.
8 Verghese A, Charlton B, Kassirer JP et al. Inadequacies of physical examination as a cause of medical errors and adverse events: a collection of vignettes. Am J Med 2015; 128: 1322-24.e3.
9 Wang JK, Ouyang D, Hom J et al. Characterizing electronic health record usage patterns of inpatient medicine residents using event log data. PLoS One 2019; 14: e0205379.
10 Kadakia KC, Hui D, Chisholm GB et al. Cancer patients’ perceptions regarding the value of the physical examination: a survey study. Cancer 2014; 120: 2215-21.
11 Kaptchuk TJ, Kelley JM, Conboy LA et al. Components of placebo effect: randomised controlled trial in patients with irritable bowel syndrome. BMJ 2008; 336: 999-1003.
12 Sinsky CA, Willard-Grace R, Schutzbank AM et al. In search of joy in practice: a report of 23 high-functioning primary care practices. Ann Fam Med 2013; 11: 272-78.
13 Patel RS, Bachu R, Adikey A et al. Factors related to physician burnout and its consequences: a review. Behav Sci (Basel) 2018; 8: 98.
14 Hurwitz B. Urban observation and sentiment in James Parkinson’s Essay on the Shaking Palsy (1817). Lit Med 2014; 32: 74-104.
15 Dolev JC, Friedlaender LK, Braverman IM. Use of fine art to enhance visual diagnostic skills. JAMA 2001; 286: 1020-21.
16 Berk SL VA. General Appearance. In: Walker HK HW, Hurst JW, ed. Clinical Methods: The History, Physical and Laboratory Examinations. 3rd ed. Boston: Butterworths; 1990.
17 McGee S. Evidence-Based Physical Diagnosis. Philadelphia, PA: Elsevier; 2018.
18 Garibaldi BT, Olson APJ. The hypothesis-driven physical examination. Med Clin North Am 2018; 102: 433-42.
19 Garibaldi BT, Russell SW. Strategies to improve bedside clinical skills teaching. Chest 2021.
20 Elder AT, McManus IC, Patrick A et al. The value of the physical examination in clinical practice: an international survey. Clin Med (Lond) 2017; 17: 490-98.
21 Garibaldi BT, Kugler J, Goyal A et al. The physical examination, including point of care technology, is an important part of the diagnostic process and should be included in educational interventions to improve clinical reasoning. Diagnosis (Berl) 2019; 6: 299-300.
