Offering advice to general practitioners (GPs) through the process of active triaging rather than an appointment may benefit patients by facilitating faster specialist advice and avoiding a potentially stressful and long waiting time to be seen in an outpatient clinic with little further added value.5 Studies have already demonstrated that this method can be compatible with both patient and GP satisfaction.6,7 Active triage has been shown to have time-saving benefits6,8 and may contribute to reduction in costs.5,8 If active triage can be performed safely and satisfactorily, it could lead to greater efficiency for patients and health services.4 There are concerns that failure to see all patients referred may lead to diagnostic error and delay, leading to potential harm. Furthermore, in many circumstances the purpose of an outpatient appointment is not just to obtain the correct diagnosis, but also to provide support to the patient and their GPs in managing chronic conditions, something that a letter of advice may not be a substitute for.
There have been strong arguments for further prioritisation of the management of chronic conditions, including neurological ones, in primary care.9 GPs have a unique long-term knowledge of the patient and their social circumstances. Active triage along with an increasing culture of ‘referral for advice’ could help empower the GP in managing neurological conditions in the community.9
In our centre, primary care referrals are assessed by one of two experienced consultant neurologists who decide whether or not referrals need to be seen and, if so, where and how soon. For patients allocated to ‘advice only’, we communicate directly with GPs, explaining why we do not think they need to be seen and offer advice on the management of their patient. This is what we mean when we use the term ‘active triage’. The primary aim of giving ‘advice only’ is to improve the service for patients and GPs rather than necessarily reduce the number of patients seen. The aim of this study was to test whether this can be performed safely and with cost benefit. The study was not designed to address GP or patient satisfaction.
The study examined patients referred to neurology outpatient services from primary care within National Health Service (NHS) Lothian Health Board between January 2016 and July 2016 inclusive. Data were obtained from computerised patient notes database. The study was approved by the NHS Lothian Quality Improvement and Clinical Governance Teams.
Patients who were given ‘advice only’ had an individualised electronic letter written to their GP offering diagnostic and/or treatment advice regarding the problem with which they were referred and explaining the reason an appointment was not given. All letters included an invitation to review the triage outcome if the GP or patient found it to be unsatisfactory and included a contact telephone number. The timeframe of response to the GP letter was approximately 7–10 days. This process did not replace the ‘on-call’ service for emergency GP referrals/questions.
Referrals were included if a neurology ‘face-to-face’ appointment had been requested and the outcome was instead a letter offering ‘advice only’ with no appointment. Patients were excluded if: GP had requested advice only, appointment was already allocated, referral redirected to another secondary healthcare team/healthcare board, advice/appointment with specialist nurse allocated, those referred for tests and those with information not available/missing.
The records of the included referrals were reviewed by one of three doctors (FM, KB and LDB). Data were collected on: type of appointment requested, GP diagnosis, active triage outcome, category of referral, whether any additional information was given, neurology diagnosis given by the triaging consultant, whether the patient was seen again within 12 months and if the patient was seen again a record of the final diagnosis.
Two consultants (JS and RD) independently reviewed the records of all patients initially allocated ‘advice only’, but who were subsequently seen either in neurology or other specialty within the next 12 months. They judged the level of diagnostic error based on a modified version of previously published categories of diagnostic error (Table 1).11 For any patients where the consultants disagreed, this was discussed and consensus reached.
Table 1 Diagnostic revision adapted from Stone et al.11
|
1 | Diagnostic error | Patient referred with symptoms that were plausibly due to motor neurone disease. The diagnosis of motor neurone disease had not been considered and was unexpected at follow up |
2 | Differential diagnostic change | Patient referred with symptoms that were plausibly related to a number of conditions. Doctor suggested carpal tunnel syndrome as most likely but considered multiple sclerosis as a possibility. Investigations and further review confirmed multiple sclerosis |
3 | Diagnostic refinement | Doctor diagnosed cervical radiculopathy but at review diagnosis refined to C7 radiculopathy |
4 | Comorbid diagnostic change | Doctor correctly identified the presence of both epilepsy and nonepileptic seizures in the same patient. At follow up, one of these disorders had remitted |
5 | Prodromal diagnostic change | Patient referred with an anxiety state. At review the patient had developed dementia. With hindsight, anxiety was a prodromal symptom of dementia but the diagnosis could not have been made at the initial referral as the dementia symptoms (or findings on examination or investigation) had not developed |
6 | De novo development of organic disease | Patient was referred, symptoms suggestive of carpal tunnel syndrome. During the period of follow up, the patient developed subarachnoid haemorrhage as a completely new condition |
7 | Disagreement between doctors – without new information at follow up | Patient was diagnosed at referral with migraine and at review with medication overuse headache by a different doctor even though there is no new information. However, if both the doctors had met the patient at follow up, they would still have arrived at the same diagnosis. This would be reflected in similar divided opinion among their peers |
8 | Disagreement between doctors – with new information at follow up | Patient was diagnosed at referral with migraine and at review with cervicogenic headache by a different doctor because of new information at review. However, the first doctor seeing the patient again at follow up continued to diagnose migraine believing the cervical spondylosis to be incidental. This would be reflected in divided opinion among their peers |
|
A | No error |
B | Patient very unlikely to be harmed or management changed by delayed review |
C | Patient potentially at risk of harm from delayed review; management may have been optimised by earlier diagnosis |
D | Patient at high risk of harm to their physical health from delayed review |
Costs
Costs of outpatient appointment vs 15 min of active triage were obtained from the NHS Patient Level Information and Costing System (PLICS system).
Results
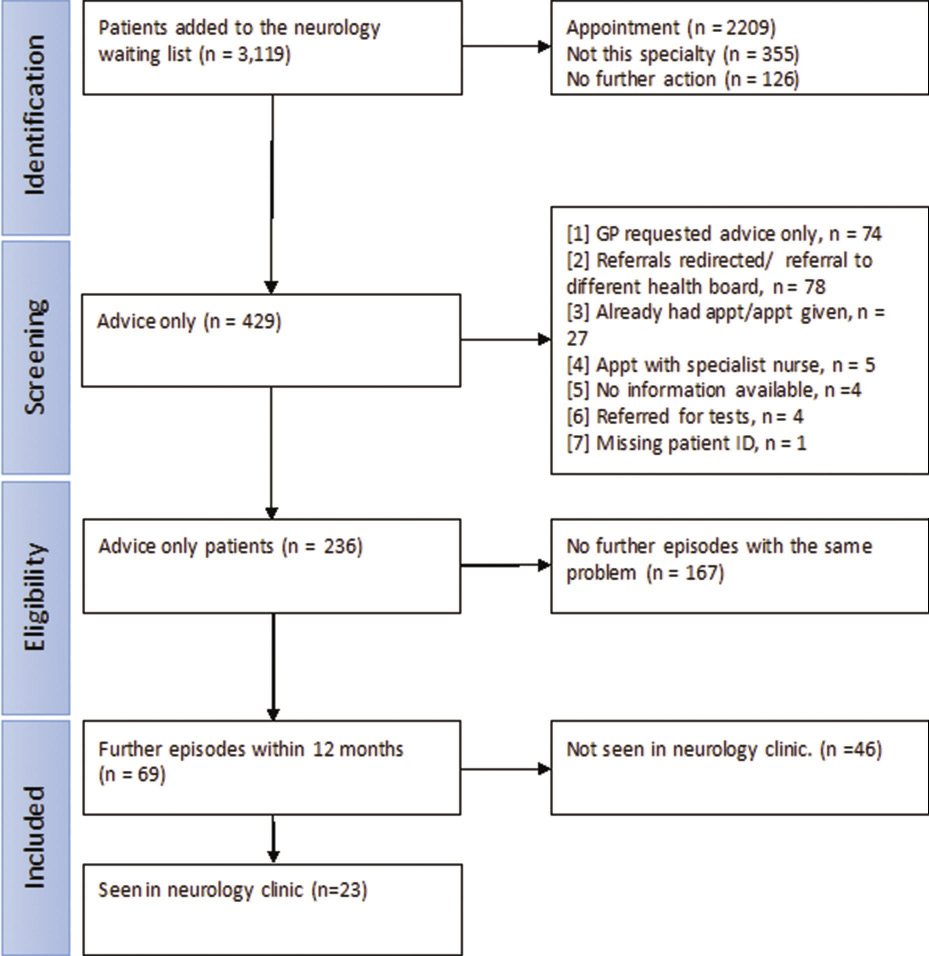
Between January 2016 and July 2016 inclusive, 3,119 patients were referred to neurology from primary care (Figure 1). Of these patients, 2,209 were suitable for an appointment, 355 were forwarded to other specialties and 126 did not require further action (e.g. the patient was already on the waiting list, or the letter was for information only). A total of 429 were coded as ‘advice only’ and their notes were reviewed. Of these, 193 referrals were excluded (Figure 1) leaving 236 referrals who were given ‘advice only’ instead of a face-to-face appointment. A total of 10% (236 out of 2,445) of patients referred for a face-to-face appointment were given advice only after active triage.
Figure 1 Identification and follow up of new neurology referrals from primary care where a face-to-face appointment was requested but written advice was offered instead. Appt: appointment
Of the 236 patients, 206 (87%) referrals were submitted by the GP as ‘routine’ and 30 (13%) as ‘urgent’. The referrals were categorised by neurological problem based on the neurology curriculum12 as follows: headache (24%), peripheral nerve (17%), spinal cord/root (14%), epilepsy and loss of consciousness (11%), sensory symptoms (9%), cranial nerves (5%), higher function and behaviour (3%), movement disorders (3%), pain (3%), functional disorders (3%) and other (9%).
In 167 (71%) referrals there were no further secondary healthcare presentations with the same problem. Of the 69 (29%) patients that did re-present, 46 patients were seen by a different specialty with the same problem and 23 were seen in neurology outpatient clinic. Some patients had multiple attendances and referrals for the same problem. The presenting problems most likely to re-present were pain (n = 6) and functional neurological problems (n = 6), with two-thirds of these patients being seen by neurology services within 12 months.
Of the 69 patients who had no further episodes with the same problem in 12 months: 61 patients had no diagnostic change when their final diagnosis was compared to that suggested by the triaging neurologist in their original advice letter. Eight patients had diagnostic revision as shown in Table 2. One patient had major diagnostic change. This final patient had been referred owing to deterioration in their known cerebellar ataxia. Initially an appointment was not given, and it was suggested referral to rehab services might be more helpful. A further letter from the GP (prior to receiving the advice letter from neurology) resulted in an appointment. Following review, the original diagnosis was revised to Huntington’s disease.
Table 2 Eight patients who had diagnostic revision following active triage
| | | |
1 | 1C | Cerebellar ataxia and pain | Huntington’s disease |
2 | 2B | Cervical radiculopathy | Brachial neuritis |
3 | 3A | Anxiety | Cognitive impairment |
4 | 3A | Peripheral neuropathy | Ulnar neuropathy |
5 | 3A | Sensory symptoms | L4/5 radiculopathy |
6 | 6A | Screening not required for cerebral aneurysm | Aneurysm in hepatic artery. May have underlying connective tissue disorder |
7 | 6B | Unknown | Sarcoidosis |
8 | 7A | Carpal tunnel syndrome | Cervical radiculopathy |
In NHS Lothian, one face-to-face appointment is costed at £129 and is allocated 30 min. Whereas, in this same time frame ‘advice only’ can be given to 10 patients at a cost of £12.90 each. This is a difference of £27,400 over the 6-month period. However, as 26 patients were eventually seen in the neurology clinic this reduces any saving to £24,046. This figure does not account for cost saving in return appointments or investigation. It also does not take into account costs if patients are then seen in other departments.
Discussion
The traditional relationship between referral from primary to secondary care has been based on a face-to-face assessment in hospital. However, changing patient expectations, service demands and availability of health information changes challenge this relationship. In our region primary care doctors told us that they wanted to promote culture of ‘referral for advice’, partly to reduce unnecessary appointments, but also to empower primary care and patients to speed up decision-making and treatment.
Our study shows that such an approach can be used safely, at least for a small proportion of patients, even in a specialty such as neurology that commonly requires face-to-face history and examination to make a diagnosis. A total of 70% of referrals given ‘advice only’ were not seen again with the same problem within 12 months. The most common presenting complaints given ‘advice only’ were headache, peripheral nerve and spinal problems. The two presenting problems given ‘advice only’ but most likely to require further neurology input within 12 months were pain and functional disorders. On analysis of patient safety only one patient had major diagnostic change following delayed review. The delay in this diagnosis was only felt to have a minor degree of harm to the patient as no new management options were available. We conclude that, given there is a base rate of diagnostic error even in patients who do attend an appointment, the ‘advice only’ response can be safely applied to neurology services.11
We did not measure GP or patient satisfaction in this study. While there were rare occasions when some GPs expressed frustration with having a referral returned, there were a similar number of episodes when GPs were positive about receiving a diagnosis and pragmatic advice earlier rather than waiting months for an appointment. One UK-based study found that 80–91% of patients and 51–89% of GPs preferred the ‘advice only’ system.7
The proportion of referrals saved was roughly equivalent to a half-time consultant neurologist.
There was a difference in the presenting complaint of patients given advice in the active triage clinic and those seen in face-to face outpatient appointments. In face-to-face outpatient appointments the most common presenting complaints are: headache, functional/psychological disorders and epilepsy.13,14 We found that some neurological conditions, such as meralgia paraesthetica and ulnar nerve paraesthesia, can be recognised more easily from a GP referral letter than others (example case shown in Box 1). We have collected some of these disorders, along with information sheets at a free website: www.neurodiagnosis.org, which may be of help to readers.
Box 1 Referral with presenting complaint of numbness to the left anterior thigh
| GP referral: Dear Colleague, I would be grateful for your opinion on this 38-year-old man who presents with a 1-year history of altered sensation in his lateral thigh. For some time now he has had reduced sensation to touch and temperature in this area. He has not noticed any back pain, or weakness. He works as a postman and finds no limitation to his daily routine. He does sometimes notice some pain and a shock like sensation in the same area. On examination, the area causing the problem is in keeping with the distribution of lateral cutaneous nerve of the thigh. He has no lower limb weakness or incoordination. He has some tenderness over the left greater trochanter but good range of movement of both hips. I would be grateful for your opinion in view of the duration of his symptoms. We are arranging routine bloods including B12/folate. I wonder if he requires any further investigation such as MRI/conduction studies. Many thanks. Neurology consultant ‘advice only’ response: I received Dr X’s recent referral, and her description sounds entirely typical for meralgia paraesthetica. He does not require any investigations apart from a blood glucose, and neither imaging nor neurophysiology contributes anything to this diagnosis, which is entirely clinical. There is no specific treatment (many patients are rather overweight, and losing weight might be helpful if this is relevant). If pain is a major issue (which seems not to be the case from your letter), then some patients may benefit from neuropathic pain drugs, and occasionally nerve blocks are used with variable success, but usually the treatment is entirely conservative with appropriate reassurance. I do not think a neurology outpatient appointment would add much more so I am not going to appoint him. I hope the above is helpful, but if not please come back to me via letter, email or telephone. I enclose a fact sheet. |
It was notable that there were cases where attempts at avoiding an appointment failed, and may have even led to more investigations and appointments than if they had seen a neurologist to begin with. An example case is shown in Box 2.
Box 2 Referral with presenting complaint of headache where active triage created more appointments rather than less
| General practitioner (GP)referral letter states that a patient has a 5-week long headache. It is described as the same as the patient’s usual migraines with typical visual aura, however, it was lasting longer. The letter queried whether a CT scan would be useful. The triaging consultant wrote an ‘advice only’ response stating that it was common for an episodic migraine to turn into chronic daily headache, especially with analgesia overuse. It was explained that a CT scan can be requested from general practice if it was felt that the benefits were felt to outweigh the risks. An information leaflet about chronic daily headache was also given. The GP referred for a CT that demonstrated a Chiari malformation. This prompted two face-to-face appointments with neurosurgery and neurology. Neurosurgery felt that the Chiari malformation was incidental and neurology gave the diagnosis of a migraine or analgesic overuse headache. This is the same diagnosis given in the triage advice letter. |
Secondary care appointments are of course about much more than just diagnosis and treatment. Many patients with complex or chronic presentations, perhaps especially those with pain and functional neurological problems who were most likely to re-present, may be referred because the GP requires support for multiple possible reasons. In contrast, sometimes referrals are made primarily because the patient has requested an opinion, which the GP may themselves not see as necessary, a view that can be reinforced by a supportive and individual letter from secondary care.
Our findings of the benefits of the ‘advice only’ system concur with the literature. Patterson et al.6 found that 45% of referrals from GPs could be managed by email advice alone and 12% by advice plus investigations. A survey of GP satisfaction with the service was high. It was estimated that 44% of a specialist neurologist’s time was saved compared with the conventional consultation. In a measure of safety, it was found that no deaths or significant changes in diagnosis were recorded. A second follow-up study of the same patient group demonstrated the safety of the ‘advice only’ approach.6 Our time and cost calculations are simplistic and do not account for a number of relevant factors (including patients being seen by other departments, return appointments, further investigations and administrative costs), but, despite this, appear promising.
An issue we did not address or standardise was whether to send all advice letters to both GP and patient. In some cases, this seemed appropriate, but in other, more complex cases and particularly those with psychiatric comorbidity, we judged that it may be better for the GP to explain the outcome of the referral to the patient. It has been suggested in a recent report by the Chief Medical Officer for Scotland that writing directly to the patient can enable them to have a more active role in their own care.15 This is something that requires further study.
The strengths of this study were its large cohort with adequate documentation in 99% of cases to assess outcomes following active triage. Limitations include the retrospective nature of the data collection and the lack of any data on GP or patient satisfaction. In addition, we currently only had access to the NHS secondary data and we do not have data on private healthcare or any further presentations to GP.
Promotion of a culture of ‘referral for advice’ for outpatient neurology services, and letters of advice rather than face-to-face appointments appears to be feasible and a safe way to manage a small proportion of patients. It allows more time and resources to be redirected into other consultations. In addition, it allows some patients to receive a quick response to their problem rather than waiting for an unnecessary clinic appointment. Active triaging offers the opportunity to make the primary–secondary care interface more effective in today’s demands on the NHS neurology departments.
References
1 Royal College of Physicians. Report of a working party local adult neurology services for the next decade. 2011. www.rcplondon.ac.uk (accessed 15/04/19).
2 Struhal W, Sellner J, Lisnic V et al. Neurology residency training in Europe – the current situation. Eur J Neurol 2011; 18: e36–40.
3 Royal College of Physicians. Outpatients: the future – adding value through sustainability. https://www.rcplondon.ac.uk/projects/outputs/outpatients-future-adding-value-through-sustainability (accessed 01/05/19).
4 Scottish Government. The Modern Outpatient: A Collaborative Approach, 2017 – 2020. Edinburgh: Scottish Government; 2017.
5 Patterson V, Humphreys J, Henderson M et al. Email triage is an effective, efficient and safe way of managing new referrals to a neurologist. BMJ Qual Saf 2010; 19: e51.
6 Patterson V, Humphreys J, Chua R. Email triage of new neurological outpatient referrals from general practice. J Neurol Neurosurg Psychiatry 2004; 75: 617.
7 Patterson V, Donaghy C, Loizou L. Email triage for new neurological outpatient referrals: what the customers think. J Neurol Neurosurg Psychiatry 2006; 77: 1295–6.
8 Harno K, Paavola T, Carlson C et al. Patient referral by telemedicine: effectiveness and cost analysis of an intranet system. J Telemed Telecare 2000; 6: 320–9.
9 Morrish P. The changing relationship between neurology and general practice in the UK. Br J Gen Pract 2009; 59: 599–604.
10 NHS Lothian. Ref Help Neurology. https://apps.nhslothian.scot/refhelp/guidelines/Pages/Neurology.aspx (accessed 01/05/19).
11 Stone J, Carson A, Duncan R et al. Symptoms ‘unexplained by organic disease’ in 1144 new neurology out-patients: how often does the diagnosis change at follow-up? Brain 2009; 132: 2878–88.
12 JRCPTB. Neurology Specialty. https://www.jrcptb.org.uk/specialties/neurology (accessed 18/04/19).
13 Ridsdale L, Mtandabari S, Noble A. 038 Referral patterns to neurology: past, present and future. J Neurol Neurosurg Psychiatry 2012; 83: e1.203-e1.
14 Stone J, Carson A, Duncan R et al. Who is referred to neurology clinics?—The diagnoses made in 3781 new patients. Clin Neurol Neurosurg 2010; 112: 747–51.
15 Scottish Government. Personalising Realistic Medicine: Published Online First: 2018. https://www.gov.scot/publications/personalising-realistic-medicine-chief-medical-officer-scotland-annual-report-2017-2018/ (accessed 01/05/19).
