Primary percutaneous coronary intervention (PPCI) is the first-line treatment for ST-segment elevation myocardial infarction (STEMI) in the UK.1,2,3 Between 1988 and 2018 the number of people living in Scotland aged 85 years or older has almost doubled.4 Moreover, the UK population aged over 85 years is predicted to more than double again by 2039; one in twelve people will be over the age of 85.5 With our ageing population the demand on PPCI services in older people is increasing, and is predicted to continue to rise.1,6,7,8 An estimated 12.7% of all cases of myocardial infarction (MI) in Scotland between 2015 and 2016 were in patients aged over 75 years.9 Published statistics on STEMI specifically in octogenarians and nonagenarians are scarce.
Atypical clinical manifestations can complicate the evolving clinical picture of a STEMI in older people. Older patients with STEMI are more likely to present late to hospital and receive a delayed diagnosis compared to the general adult population.10 This group are also more likely to develop cardiac complications post-STEMI, including cardiac failure, cardiogenic shock, arrhythmia and death.1,8,10,11 There is a paucity of data on the optimal treatment of STEMI in this high-risk group as they are majorly underrepresented in clinical trials.2,8,12 Despite this, the National Institute of Health and Care Excellence and the European Society of Cardiology guidelines recommend PPCI as first-line management for all patients who have a STEMI regardless of their age at presentation.13,14
The aim of our study was to evaluate real-world survival outcomes in very old patients aged 85 years or older who undergo invasive coronary angiography (ICA) assessment ± PPCI for acute STEMI.
Methods
Population and study design
We performed a retrospective observational analysis that focused on patient outcomes after ICA ± PPCI in patients aged 85 years or older. Clinical data were collected retrospectively on all patients aged 85 years or older who were referred and accepted for PPCI for treatment of STEMI at our regional cardiac catheterisation laboratory in the West of Scotland between 2013 and 2018 inclusive. For the purposes of our study, all patients aged 85 years or older were classified as ‘very elderly’. The octogenarian subgroup comprised of all patients aged ≥80 years at the time of referral for PPCI. The nonagenarian subgroup comprised of all patients aged ≥90 years. Patients did not switch groups if they exceeded the age of 89 years during follow-up.
Research database
An existing database that included the hospital identification numbers of all patients referred and accepted for PPCI in Lanarkshire during the study period was accessed via our local cardiology department. This dataset included details on patient journey, which allowed for door-to-balloon times to be calculated, and procedural characteristics. All patient-identifiable information was pseudonymised for data collection.
Inclusion and exclusion criteria
All patients aged 85 years or older with acute STEMI who were referred and accepted for PPCI during the six-year study period were screened for inclusion. Patients who did not undergo emergency angiography upon arrival to the cardiac catheterisation laboratory were excluded.
Data collection
Data on patient characteristics, morbidity, mortality and acute hospital readmissions post-STEMI were extracted from digital medical records. Our study covariates included age, gender, mobility status, smoking history, diabetes mellitus, baseline renal function (estimated glomerular filtration rate [eGFR] ml/min/1.73m2), admission haemoglobin, left ventricular function and culprit epicardial artery. Patients who required one or more mobility aid including a walking stick or a Zimmer frame were defined as patients who mobilised with assistance vs patient who mobilised independently. Mobility status was used as a marker of frailty for the purpose of this study. Smoking history was categorised as current, previous or no tobacco use. Left ventricular function was categorised as normal, mild/mild–moderate impairment, moderate/moderate–severe impairment and severe impairment. Culprit vessel identified on angiogram was categorised as left anterior descending (LAD) artery or other.
Statistical analysis
Statistical analysis was performed in RStudio for Mac OS X version 3.5.3. Categorical variables are presented as an absolute frequency and percentage. Continuous data are expressed as mean ± standard deviation for variables that were normally distributed, and as median and interquartile range (25–75th percentiles) for variables that were not distributed normally. Survival of octogenarians vs nonagenarians at 30 days and at one year post-STEMI was compared using two-tailed Fisher’s exact tests. Survival analysis was performed using Cox regression and Kaplan–Meier analysis. A value of P<0.05 was considered statistically significant.
Ethics
Following the NHS Health Research Association guidelines and the guidance from our centre, formal ethical approval was not required for completion of this study (Appendix 1a and 1b). All patient-identifiable information was removed prior to analysis.
Results
Baseline characteristics
One hundred and seventy-two patients aged 85 years or older with STEMI were referred and accepted for PPCI over the six-year study period. This was 4.8% of the total number of accepted PPCI referrals to our tertiary centre during this time. The absolute number of patients undergoing PPCI per year did not show an upward trend over the study period.
The median door-to-balloon time was 26 minutes. Eight patients (4.7%) did not proceed to emergency ICA on arrival to the cardiac catheterisation laboratory. Reasons for this were: (i) haemodynamic instability, (ii) patient refusal and (iii) absence of ST elevation on electrocardiogram (ECG). Of the 164 patients who proceeded to ICA, 122 (74.4%) were aged 85–89 years old, and 42 (25.6%) were aged ≥90 years old. One hundred and forty-three patients (87.2%) were offered PPCI. Reasons for not proceeding to PPCI were normal coronaries or no obstructive coronary disease (n=17) and haemodynamic instability (n=4). PPCI was successful in over 95% of cases. Seven patients (4.9%) died during the procedure.
The oldest patient to receive PPCI was 99 years old. Forty-two patients (25.6%) were aged 90 years or older. There was no statistically significant difference in the mean age of males and females who underwent ICA ± PPCI (87.8 vs 88.2 years, P=0.39). Median length of stay was 7 (3–11) days. The range was 1–190 days. Patient characteristics are summarised in Table 1.
Table 1 Patient characteristics
|
|
|
|
Demographic characteristics
|
|
|
Age (years)
|
88.0 ± 2.97
|
|
Female gender, n (%)
|
91 (55.5)
|
|
Cardiovascular risk factors
|
|
|
Diabetes mellitus, n (%)
|
26 (15.9)
|
|
Current tobacco use, n (%)
|
15 (9.1)
|
|
Previous tobacco use, n (%)
|
44 (26.8)
|
|
Haematological and biochemical results
|
|
|
Haemoglobin (g/dl)
|
11.8 ± 1.8
|
|
eGFR (ml/min/1.73m2)
|
51.1 ± 11.5
|
|
LV function post-MI
|
|
|
Preserved, n (%)
|
33 (20.1)
|
|
Mild/mild–moderate, n (%)
|
31 (18.9)
|
|
Moderate/moderate–severe, n (%)
|
29 (17.7)
|
|
Severe, n (%)
|
30 (18.3)
|
|
Unknown, n (%)
|
41 (25.0)
|
|
Patient hospital journey
|
|
|
Length of stay (days)
|
7 (3–11)
|
|
Independently mobile, n (%)
|
92 (56.1)
|
|
Survived admission, n (%)
|
131 (79.9)
|
|
Survivors discharged to own home, n (%)
|
124 (94.7)
|
|
Survivors discharged to nursing home, n (%)
|
7 (5.4)
|
| |
|
Survival analysis and clinical outcomes
One hundred and thirty-one patients (79.9%) survived STEMI admission. Sixty patients (45.8%) were readmitted to hospital as emergencies within the first year post-STEMI. Thirty-eight patients (29.0%) had one emergency hospital admission and 22 patients (16.8%) had two or more emergency hospital admissions. Reasons for hospital readmission within the first year post-STEMI are summarised in Table 2. Chest pain attributed to angina or non-cardiac chest pain was the most common reason for hospital readmission, followed by lower respiratory tract infections and falls.
Table 2 Primary reason for emergency hospital readmission in year one post-STEMI
|
|
|
|
Chest pain
|
21
|
|
Community-acquired pneumonia
|
15
|
|
Falls
|
13
|
|
Cardiac failure
|
10
|
|
Shortness of breath
|
7
|
|
Syncope/collapse
|
7
|
|
Acute coronary syndrome
|
4
|
|
General decline
|
4
|
|
Change in bowel habit
|
4
|
|
Sepsis
|
3
|
|
Stroke
|
1
|
|
Other
|
5
|
| |
|
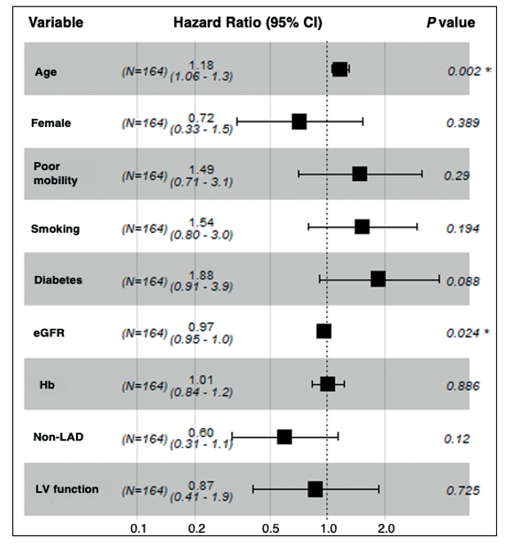
The 30-day mortality of all patients who underwent ICA ± PCI was 21.3% (n=35). One-year mortality was 33.5% (n=55). Octogenarians had better survival compared to nonagenarians at 30 days (84.4% and 61.9%, respectively, P=0.004) and at one year (62.3% and 40.5%, respectively, P=0.019). The regression coefficients, hazard ratios (HR) and corresponding 95% confidence intervals (CI) estimated for univariate Cox regression analysis between one-year mortality and study covariates are shown in Table 3. Age, mobility status, diabetes mellitus and baseline renal function were predictors of one-year mortality. A multivariate Cox regression analysis adjusting for all study covariates demonstrated that age (HR 1.14, 95% CI: 1.06–1.2, P=0.002) and baseline renal function (HR 0.97, CI: 0.95–1.00, P=0.024) were independent predictors of one-year mortality. This is illustrated by the Cox proportional hazard model in Figure 1. The model was statistically significant (P=0.01).
Table 3 Univariate Cox regression analysis of risk factors for one year mortalitya
| |
|
|
|
|
Age
|
0.13
|
1.14
(1.06–1.23)
|
P<0.001*
|
|
Female
|
–0.29
|
0.75
(0.47–1.20)
|
P=0.230
|
|
Poor mobility
|
0.63
|
1.89
(1.18–3.03)
|
P=0.008*
|
|
Diabetes
|
0.60
|
1.82
(1.05–3.15)
|
P=0.034*
|
|
eGFR
|
–0.03
|
0.97
(0.95–0.99)
|
P=<0.001*
|
|
Haemoglobin
|
0.10
|
1.11
(0.97–1.26)
|
P=0.131
|
|
Smoking
|
0.23
|
1.26
(0.76–2.10)
|
P=0.374
|
|
Non-LAD
|
–0.15
|
0.86
(0.53–1.42)
|
P=0.564
|
|
LV Impairment
|
0.22
|
1.35
(0.67–2.33)
|
P=0.483
|
Figure 1 Cox proportional-hazards regression model to determine risk factors of one-year mortality in patients aged ≥85 years with STEMI. The model is adjusted for study variables age, gender, mobility status, diabetes mellitus, smoking, left ventricular (LV) function (%), haemoglobin (Hb), eGFR and culprit vessel (LAD vs non-LAD). Increasing age and eGFR were independent predictors of one-year mortality.
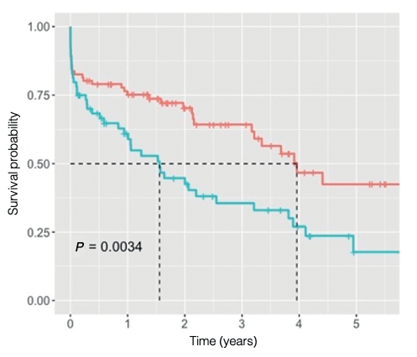
Median survival of all patients was 2.55 years. There was no statistically significant difference in median survival between males and females (P=0.322). The median survival of octogenarians and nonagenarians was 3.68 years and 1.06 years, respectively (P=0.009). The median survival of independently mobile patients and patients who mobilised with assistance was 3.96 years and 1.56 years, respectively (P=0.003). Kaplan–Meier analysis in Figure 2a illustrates the survival probability of all patients. Figure 2b compares survival of octogenarians and nonagenarians, and Figure 2c compares survival of independently mobile patients and patients who mobilised with assistance.
Figure 2a Long-term survival of patients aged ≥85 years following angiography ± PPCI. Survival probability of all patients who underwent emergency angiography ± PPCI over five years post-STEMI. Median survival time (dashed lines) was 2.55 years.
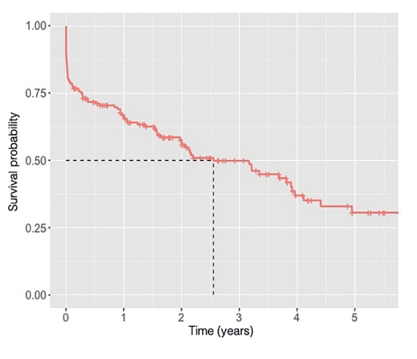
Figure 2b Long-term survival of all patients aged ≥85 years following angiography ± PPCI categorised by age. Survival probability of octogenarians (red = 85–89 years) compared to survival of nonagenarians (blue = ≥90 years) over five years post-STEMI. Median survival time (dashed lines) in octogenarians and nonagenarians was 3.68 years and 1.06 years, respectively.
Figure 2c Long-term survival of all patients aged ≥85 years following angiography ± PPCI categorised by mobility status. Survival probability of patients who mobilised independently (red) compared to patients who mobilised with assistance (blue) over five years post-STEMI. Median survival time (dashed lines) in patients who mobilised independently and patients who mobilised with assistance of a mobility aid was 3.96 years and 1.56 years, respectively.
Discussion
Multi-morbidity and frailty are becoming exceedingly recognised and diagnosed in our ageing population. The estimated average life expectancy of an 85-year-old in Scotland between 2011 and 2017 was 5.6 years and 6.4 years for males and females, respectively.9 Median survival of STEMI patients treated with PPCI in this analysis was just under half of this (2.55 years). The mean estimated mortality rate of the general Scottish population aged 85 years or older from 2013 to 2018 was 15.9% per year.9 The one-year mortality in our study population exceeded slightly double this (33.5%). In addition to increasing age, our study found that impaired renal function was an independent predictor of one-year mortality. This indicates that renal dysfunction in older people is a proxy for multi-morbidity and reduced physiological reserve to deal with the insult of a STEMI. This is supported by data from previous studies investigating post-PCI outcomes in the elderly.1
In other observational studies looking at PPCI in the over-80s, the percentage range of all STEMI presentations was 8–20%. Our study percentage was lower than this range (4.8%), which is likely due to higher age criteria. These studies had 30-day and one-year mortality ranges of 17–21% and 20–28%, respectively.1,7,8,15 The figures noted in our study were both higher than these ranges (21.3% and 33.5%, respectively). These results could again be explained by the older age criteria used for our study.
A recent study by Steele et al. sought to establish an association between socioeconomic status and survival outcomes post-PPCI for STEMI. This study found that the 30-day and one-year mortality rates in the more deprived socioeconomic status quartiles were 30.5–37.1% and 29.9–34.6%, respectively.16 Only 3% of their total study population were aged 85 years or older. Although no direct comparison from these figures can be drawn, we can observe that the 30-day mortality of our very old study population was lower than this range, and one-year mortality was within this range.
With regards to hospital readmissions post-STEMI, our study found that under half of patients (45.8%) was readmitted to hospital within the first year with an acute medical problem. The most common reason for emergency readmission was chest pain attributed to angina or non-cardiac chest pain rather than an acute coronary syndrome. A study on post-MI outcomes by Andres et al. found slightly lower readmission rates in the first year in patients older than 75 years (38% vs 45.8%), but higher readmission rates in patients under 45 years (50% vs 45.8%).17 Despite age-related decline, the relatively disease-free longevity in elderly patients selected to receive PPCI may lead to better prognoses post-STEMI relative to middle-aged adults with high-risk factor profiles who develop cardiac disease early on in life.
Taking into account poor baseline prognostic indicators and post-STEMI morbidity and mortality, this poses a complex ethical question for cardiologists treating STEMIs in old and very old patients in routine clinical practice. There is a lot of ambiguity surrounding whether or not expensive and invasive treatments should be offered to the very old because a strong evidence base to support these treatments in this subgroup of the population is lacking. This is primarily due to the limited numbers of very old patients included in randomised controlled trials. This is particularly true of studies on invasive management using coronary revascularisation, which becomes immediately pressing in the context of acute STEMI. A retrospective study of a relatively small British dataset of over 400 PPCI cases revealed a significant one-year mortality difference between patients under 60 of 5.4% compared to 24.6% in those over 80.18 The After Eighty study, a seminal trial that investigated whether patients aged 80 years or older with non-STEMI or unstable angina had a reduced risk of major adverse cardiac events (MACE) with interventional therapy versus pharmacological therapy. This study demonstrated that patients managed conservatively were at increased risk of MACE at median follow-up of 1.53 years (HR 0.53, P=0.0001).19 Whilst it is appropriate to manage very old patients conservatively in some cases, our findings demonstrate that very old patients benefit from PCI. Fifty per cent of all patients survived for more than 2.5 years, and over three-quarters of our study population survived STEMI hospital admission, of which 95% were discharged to their own home and were able to live independently. Although age is important, our results have highlighted that it is not the only identifiable factor that significantly impacts outcomes. In an ideal scenario, a combination of parameters, available to paramedics, would facilitate risk stratification for PPCI outcome. Given the time sensitive nature of PPCI, a comprehensive geriatric assessment would be unfeasible. Mobility status is a subjective component of the Rockwood Clinical Frailty Scale, a quick clinical screening tool used to identify frailty. In this study, mobility status was used as a proxy for frailty. Our regression model highlighted that impaired mobility status corresponded with poorer outcomes. This suggests that a frailty assessment prior to referral could aid determination of best PPCI candidates. Mobility status, like age, is readily available to paramedical colleagues. A combination of age and mobility status could be feasibly used in a risk stratification process prior to PPCI acceptance. However, given this is a retrospective study, it is not possible to determine the absolute weight of impact on outcomes that each of these parameters has.
One of the major limitations of our study was that it was limited to patients who were accepted and transferred to the cardiac catheter laboratory for assessment. This study was therefore unable to capture all patients with STEMI aged 85 years or older during the study period. As a consequence, a comparative analysis between patients managed conservatively for STEMI and those who received revascularisation therapy was not possible. Other limitations included a small sample size of our study population and missing data due to missing and incomplete copies of electronic medical records following patient discharge.
In conclusion, whilst a personalised cardio-geriatric approach should still be applied to guide PCI decision-making in older people, our data supports PPCI as first-line treatment for STEMI in patients aged 85 years and older. Despite long hospital stays and high one-year mortality rate, the majority of patients in our study were discharged to their own homes, and half of patients survived for more than two and a half years. This demonstrates that there are potentially good quality life years to be gained following emergency revascularisation. Advanced age should therefore not be used as an exclusion criterion in isolation for PPCI, and PPCI should be offered routinely to all older patients with STEMI. With projected figures of our UK population aged 85 years and older to more than double within the next 20 years, a robust evidence base is needed to support our findings.
References
- Bromage DI, Jones DA, Rathod KS et al. Outcome of 1051 Octogenarian patients with ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention: observational cohort from the London Heart Attack Group. J Am Heart Assoc 2016; 6: 1–11.
- Bueno H, Betriu A, Heras M et al. Primary angioplasty vs fibrinolysis in very old patients with acute myocardial infarction: TRIANA randomized trial and pooled analysis with previous studies. Eur Heart J 2010; 32: 51–60.
- Gao L, Hu X, Liu Y et al. Percutaneous coronary intervention in the elderly with ST-segment elevation myocardial infarction. Clin Interv Aging 2014; 9: 1241–6.
- National Records of Scotland. Mid-2018 population estimates. www.nrscotland.gov.uk/statistics-and-data/statistics/statistics-by-theme/population/population-estimates/mid-year-population-estimates/mid-2018 (2018, accessed 16 July 2019).
- Office for National Statistics. National Population Projections: 2014-based Statistical Bulletin. www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/popul... (2014, accessed 8 October 2019).
- Dangas GD, Singh HS. Primary percutaneous coronary intervention in octogenarians: navigate with caution. Heart 2010; 96: 813–4.
- Claessen BEPM, Kikkert WJ, Engstrom AE et al. Primary percutaneous coronary intervention for ST elevation myocardial infarction in octogenarians: trends and outcomes. Heart 2010; 96: 843–7.
- Caretta G, Passamonti E, Pedroni PN et al. Outcomes and predictors of mortality among octogenarian and older with ST-segment elevation myocardial infarction treated with primary coronary angioplasty. Clin Cardiol 2014; 37: 523–9.
- National Records of Scotland. Age-standardised death rates calculated using the European Standard Population. www.nrscotland.gov.uk/statistics-and-data/statistics/statistics-by-theme/vital-events/deaths/age-standardised-death-rates-calculated-using-the-esp (2018, accessed 16 July 2019).
- Goch A, Misiewicz P, Rysz J et al. The clinical manifestations of myocardial infarction in elderly patients. Clin Cardiol 2009; 32: E46–51.
- Hafiz AM, Jan MF, Mori N et al. Contemporary clinical outcomes of primary percutaneous coronary intervention in elderly versus younger patients presenting with acute ST-segment elevation myocardial infarction. J Interv Cardiol 2011; 24: 357–65.
- Boer SPM, Westerhout CM, Simes RJ et al. Mortality and morbidity reduction by primary percutaneous coronary intervention is independent of patient’s age. JACC Cardiovasc Interv 2010; 3: 324–31.
- National Institute for Health and Care Excellence. Myocardial infarction with ST-elevation: acute management. www.nice.org.uk/guidance/CG167 (2013, accessed 19 July 2019).
- European Society of Cardiology. Acute myocardial infarction in patients presenting with ST-segment elevation (Management of) Guidelines. www.escardio.org/Guidelines/Clinical-Practice-Guidelines/Acute-Myocardial-Infarction-in-patients-presenting-with-ST-segment-elevation-Ma (2017, accessed 19 July 2019).
- Antonsen L, Jensen LO, Terkelsen CJ et al. Outcomes after primary percutaneous coronary intervention in octogenarians and nonagenarians with ST-segment elevation myocardial infarction: From the Western Denmark heart registry. Catheter Cardiovasc Interv 2013; 81: 912–9.
- Steele L, Palmer J, Fotheringham J et al. Impact of socioeconomic status on ST-elevation myocardial infarction in a universal healthcare system. Int J Cardiol 2019; 276: 26–30.
- Andres E, Cordero A, Magan P et al. Long-term mortality and hospital readmission after acute myocardial infarction, an eight-year follow-up study. Rev Esp Cardiol 2012; 65: 414–20.
- Sharma V, Srinivasan M, Smith D. Age and outcomes of primary percutaneous intervention for ST elevation myocardial infarction in a tertiary centre – are we there yet? J Geriatr Cardiol 2015; 12: 263–9.
- Tegn N, Abdelnoor M, Aaberge L et al. Invasive versus conservative strategy in patients aged 80 years or older with non-ST-elevation myocardial infarction or unstable angina pectoris (After Eighty Study): an open-label randomised controlled trial. Lancet 2016; 387: 1057–1065.