A 77-year-old male was admitted with shortness of breath on exertion due to heart failure, on a background of cerebral amyloid angiopathy diagnosed following transient ischaemic attacks due to amyloid spells, previous right middle cerebral artery infarct and ischemic heart disease.
On admission he was alert and orientated; however, he later became confused and agitated, without focal neurology. Computed tomography (CT) scan of the brain revealed an acute intracerebral haemorrhage originating from the left inferior frontal lobe with intraventricular extension to the lateral and third ventricle extending into the cerebral aqueduct with obstructive hydrocephalus (Figure 1). He became comatose with a Glasgow Coma Scale (GCS) score of 4/15. Conservative management was advised because of the patient’s age, co-morbidities and extent of the haemorrhage. Supportive management and palliative measures were initiated.
Figure 1 CT brain of the patient. (1) On the left, showing acute intracranial haemorrhage that has extended to the lateral and third ventricle. The blue arrow denotes blood obstructing the aqueduct of Sylvius. Hydrocephalus is also evident. (2) On the right, resolving hydrocephlus with the arrow showing resolution of the clot in the aqueduct.
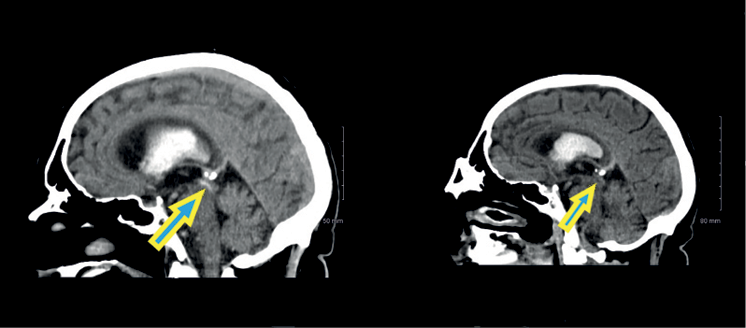
Two days later the patient spontaneously awoke returning to GCS 14. A repeat CT brain revealed resolution of the blood in the aqueduct with complete decompression of the hydrocephalus. The patient required rehabilitation and later returned home close to his baseline level of function with some residual cognitive impairment.
Cases of spontaneous resolution of this condition in adults have been rarely reported.1–5 It has been hypothesized that it probably occurs when the fourth ventricle is absent of blood with minimal haemorrhage in the cerebral aqueduct, allowing the increased intracranial pressure to push the blood clot downwards, thus resolving the hydrocephalus.
We report a rare phenomenon of spontaneous decompression of obstructive hydrocephalus secondary to blood in the cerebral aqueduct. It has seldom been reported in adults. It is important to be aware of its possibility when managing hydrocephalus due to aqueduct thrombotic occlusion. 
