Shielding, use of masks and hand hygiene: could this be the answer to winter pressures?
The Department of Health issued shielding guidelines for clinically extremely vulnerable (CEV) members of the population during the COVID-19 pandemic. Along with shielding, hand hygiene and face masks have also been used extensively. These measures have also had a dramatic impact in reducing admissions due to other chronic respiratory conditions.
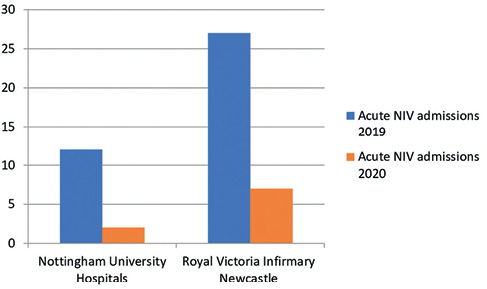
We surveyed 603 long-term ventilation (LTV) patients in two large centres, Nottingham University Hospitals and Newcastle upon Tyne Hospitals, about shielding, and 86.6% reported observing strict adherence to shielding. Of those surveyed, 30 (5%) reported having developed COVID-19 symptoms but only two (0.33%) tested positive with none requiring admission. Figure 1 shows comparative retrospective data from our LTV patients demonstrating a 76% reduction in hospital admissions between March to June 2019 and 2020. Similarly, a 37% reduction was also observed in all-cause acute NIV admissions (54 in 2019 to 34 in 2020). These reductions are superior to what can be achieved by pulmonary rehabilitation (33%)1 or by using combined inhaler therapy for COPD (24%).2 It is likely that these vulnerable patients were trying to avoid hospital admission, but it would be difficult to be treated in the community for severe hypercapnic respiratory failure requiring non-invasive ventilation.
Figure 1 Hospital admissions in patients on LTV
During winter months there is a surge in admissions due to influenza and other respiratory viral infections every year. For example, there were roughly 360 admissions a week in February 2019 due to influenza.3 In addition, several patients acquire these infections in hospital. The net effect is a lack of bed capacity, cancellation of surgical procedures, including cancer-related operations, and ultimately avoidable deaths. Influenza and indeed other respiratory viruses have a similar mode of transmission to the SARS-CoV-2 virus, and measures used against COVID-19 are likely to be effective against these infections. However, as over the decades we have become familiar with these infections, very few preventative measures except for vaccination (which has limited effectiveness) are practised.
One possible drawback of shielding is its psychosociological and economic impact. UK national data showed that 95% of 2.2 million CEV people reported either completely or mostly following government shielding guidance,4 with 61% reporting no difference in their mental health and wellbeing since the start of shielding. Also, 72% of CEV people were not in employment and most did not live with children, making it easier to shield. Of those in employment, a proportion will now be able to work remotely, further reducing the economic impact of shielding.
Adopting a blanket strategy to shield all patients with chronic respiratory illness during winter is impractical. However, a stratified shielding of CEV people can be adopted taking into consideration its impact on their mental health and personal finances. Social distancing measures particularly during winter months, hand hygiene, universal use of masks and point-of-care testing for respiratory viruses would further reduce disease transmission and improve health outcomes. This in turn would ease the perpetual winter pressures on the NHS as well.
Michael Avoseh1, Ben Messer2, Alison Armstrong2, Milind Sovani1
1Department of Respiratory Medicine, Nottingham University Hospitals
2Newcastle upon Tyne Hospitals NHS Foundation Trust, North East Assisted Ventilation Service
Department of Respiratory Medicine, Kings Mill Hospital, Mansfield Rd, Sutton-in-Ashfield NG17 4JL
Email: michael.avoseh@nhs.net
doi: 10.4997/JRCPE.2021.223
References
1 Hein I. Pulmonary rehab reduces COPD readmissions. Medscape 18 Aug 2020. https://www.medscape.com/viewarticle/935873.
2 National Institute for Health and Care Excellence (NICE). Resource impact report. Chronic obstructive pulmonary disease in over 16s: diagnosis and management (update) (NG115). https://www.nice.org.uk/guidance/ng115/resources/resource-impact-report-pdf-6602803741.
3 https://www.gov.uk/government/statistics/weekly-national-flu-reports-2018-to-2019-season.
4 https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/... andshieldingofclinicallyextremelyvulnerablepeopleinengland/ 28mayto3june2020.
COVID-19 vestibular neuritis (CVN) in a healthcare worker: a rare complication of COVID-19 infection
Covid-19 disease caused by SARS-CoV-2 virus was declared a pandemic by the World Health Organization (WHO) and cases continue to increase worldwide to date.1 Though COVID-19 is primarily a respiratory disease, other rare presentations like acute abdomen, thromboembolism, cardiomyopathy and cerebrovascular events have been reported.2 We report a unique case of COVID-19-associated vestibular neuritis in a healthcare worker (HCW).
A 38-year-old male medical professional presented with intermittent fever, myalgia and watery loose stools, eight days after completing clinical duties in a COVID-19 ward. He was a non-smoker, non-alcoholic, with no history of diabetes mellitus, hypertension or any other comorbidities. His hydration, vitals and systemic examination were unremarkable. An RT-PCR testing on nasopharyngeal swab for COVID-19 on day one of symptoms came positive. All the septic, inflammatory coagulation markers, including hemogram, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), ferritin, d-dimer, fibrinogen and platelet count, were within normal limits. He was given symptomatic treatment with oral rehydration solution, antipyretics, probiotics and vitamin C. He became afebrile and loose stools subsided within two days. After four days of afebrile period, he developed acute vertigo with nausea and vomiting. Vertigo symptoms were worse with head movement and in erect posture. Nystagmus was present on turning his head side to side. A hearing test was normal. A Romberg’s test was negative with eyes open and closed. There were no focal neurological deficits. Systemic examination was normal. A CT chest scan was reported as CO-RADS 2 and a chest X-ray showed features of subtle air space opacities and prominent bronchovascular markings consistent with mild resolving viral pneumonia. A diagnosis of COVID-19 vestibular neuritis (CVN) was considered. He was treated with tablets of hydroxychloroquine (200 mg BD), dexamethasone (6 mg BD) and low-molecular-weight heparin (LMWH) (40 mg, SC OD) for five days. He also received betahistine (24 mg/day), following which his symptoms improved gradually. He received vestibular rehabilitation therapy during follow-up. It took four weeks for complete resolution of symptoms, following which betahistine was tapered and stopped.
Vestibular neuritis is a benign, self-limiting condition presenting with vertigo, nystagmus, nausea, vomiting and abnormal gait. It is often an acute viral or postviral inflammatory disorder due to the involvement of the vestibular segment of the eighth cranial nerve. It is a diagnosis of exclusion, made only when other vertigo causes like stroke and central lesions are ruled out. Though self-limiting, symptoms during an acute phase can be severe and crippling.3
A literature search revealed another similar case of CVN reported in a 29-year-old woman who presented with acute vertigo, which settled within one week of antiviral, steroid and symptomatic treatment.2 However, in our case, vertigo developed after an acute febrile phase and gradually resolved over four weeks. The treatment of CVN consists of acute symptomatic treatment with medications such as anti-emetics, antihistamines and benzodiazepines. The role of steroid therapy is inconclusive.2,3 Vestibular rehabilitation with physical exercises and balance training hastens recovery. Audiovestibular symptoms in COVID-19 are extremely rare (1%) and long-term consequences such as audiovestibular dysfunction have not been reported.4 Clinicians should be aware of CVN for early diagnosis and management.
Thirunavukkarasu Arun Babu1, Manuj Kumar Sarkar2, Vijayan Sharmila3
1Associate Professor, 2Associate Professor of General Medicine, 3Additional Professor
All India Institute of Medical Sciences (AIIMS), Mangalagiri, Andhra Pradesh, India
Email: babuarun@yahoo.com
doi: 10.4997/JRCPE.2021.224
References
1 Sharmila V, Babu TA, Balakrishnan P. Optimizing telemedicine for providing obstetric and reproductive health care services during COVID-19 pandemic. Int J Community Med Public Health 2020; 7: 3278–83.
2 Malayala SV, Raza A. A case of COVID-19-induced vestibular neuritis. Cureus 2020; 12: e8918. doi: 10.7759/cureus.8918.
3 Le TN, Westerberg BD, Lea J. Vestibular neuritis: recent advances in etiology, diagnostic evaluation, and treatment. Adv Otorhinolaryngol 2019; 82: 87–92.
4 Almufarrij I, Uus K, Munro KJ. Does coronavirus affect the audio-vestibular system? A rapid systematic review. Int J Audiol 2020; 59: 487–91.
It is all about who you know: disparities in opportunity
Academic output varies significantly between institutions, as does exposure to formal, experienced academic guidance and mentorship. A recent study conducted at the University of Oxford by Mashar et al.1 highlighted the need for greater equity and balance in research. National medical student interest in pursuing integrated academic training is currently heavily skewed towards institutions with research components inherently incorporated into undergraduate curricula.1 Only a selection of UK universities currently mandate higher degree acquisition in the form of intercalating, which often presents an integral stepping stone into research interest and professional academic growth.2 Given these disparities in opportunity and support, it is time to work collaboratively to facilitate national personalised networks of guidance for academically enthused students and trainees.
Mentorship in academia provides notable influence on juniors’ career trajectories and productivity in research in the form of publications and grant achievements.3 Despite evidence that such guidance nurtures success, most medical schools and postgraduate training programmes are yet to implement academic supervisors as, at the very least, a non-compulsory option. This could serve as one potential intervention for institutions to provide greater guidance and opportunity.
Nationally recognised and respected societies like the National Student Association of Medical Research (NSAMR) have already taken initiative in recent years, by creating mentoring networks for students interested in research.4 Systematic, well-structured and collaborative frameworks need further development and implementation nationally for medical students and junior trainees to provide greater balance in opportunity across all institutions, genders and ethnic groups.
Sofian Youssef
Academic Surgery Foundation Doctor
University of Nottingham, Nottingham, NG7 2RD
Email: sofian_y@hotmail.co.uk
doi: 10.4997/JRCPE.2021.225
References
1 Mashar M, Kilgour J, Nanapragasam H et al. Academic medicine: the continuing challenges. Clin Teach 2020; 17: 81–5.
2 Philip AB, Prasad SJ, Patel A. Should an intercalated degree be compulsory for undergraduate medical students? Med Educ Online 2015; 20: 29392.
3 Sambunjak D, Straus SE, Marusić A. Mentoring in academic medicine: a systematic review. JAMA 2006; 296: 1103–15.
4 National Student Association of Medical Research. NSAMR mentorship: guiding you to success. https://nsamr.ac.uk/mentorship.
Are aptitude tests the solution to widening participation during COVID-19?
Smith and Cleland’s paper was particularly insightful as it addressed an age-old problem, widening participation in medicine, within the new context of COVID.1 As a medical student who attended a state school, I appreciate how the authors have highlighted the potential problems facing medical applicants this year. However, I would like to challenge their suggestion that aptitude tests, such as the UCAT, should be given greater weighting during the admissions process.
They argue that evidence suggests that these tests are better predictors of medical school performance and are less influenced by socioeconomic class than school examinations.1 Unfortunately, a recent study found contradictory effects and no studies have investigated the impact of COVID-19 on these aptitude tests.2,3 It is plausible to assume the impacts on education identified by Smith and Cleland may also negatively affect students’ ability to access and prepare for these aptitude tests, minimising any potential benefit of their use. The recent problems experienced by final-year medical students sitting the online situation judgement test are a clear example of this.4
While many of Smith and Cleland’s points are strong, medicine admissions boards should use the UCAT with caution this year and refrain from increasing its weighting. Instead, admissions boards should understand the individuality of each application and judge applicants based on their personal and educational context.
Luke Cameron Read
MBBS and MClinEd Student
Norwich Medical School, University of East Anglia, Norwich NR4 7TJ
Email: Luke.Read@uea.ac.uk
doi: 10.4997/JRCPE.2021.226
References
1 Smith KG, Cleland J. Drastic times need drastic measures: COVID-19 and widening access to medicine. J R Coll Physicians Edinb 2020; 50: 431–435.
2 Griffin B, Horton GL, Lampe L et al. The change from UMAT to UCAT for undergraduate medical school applicants: impact on selection outcomes. Med J Aust 2021; 214: 84–89.
3 Powis DA, Munro D, Bore MR. Is the UCAT appropriate for selecting undergraduate medical students? Med J Aust 2021; 214: 77–78.
4 Nabavi N. BMA calls for urgent review of online exam for medical students. BMJ 2021; 372.
Authors’ reply
We thank Read for his positive comments on our paper ‘Drastic times need drastic measures’.1 Read echoes our plea for a holistic approach to medical school selection (often referred to as contextualised admissions). He is less supportive of our other suggestion, that aptitude tests, such as the UCAT (previously known as UKCAT), could be given greater weighting in admissions processes during COVID-19 admission. He questions the evidence that aptitude tests generally are less influenced by socioeconomic class than is school performance.
In respect to the weighting of UCAT, Read cites a recent Australian study by Griffin et al.2 and a commentary on that same study as evidence.3 The Griffin et al. study is among the first published data since UCAT replaced UMAT in Australia. This valuable paper highlighted that the influence of socioeconomic class on performance is similar for UMAT and UCAT (i.e. UCAT is no worse, or no better, than another aptitude test in this respect).
In respect to Read’s second point, Griffin and colleagues did not look at the associations between UCAT, socioeconomic factors and medical school performance. However, others have done so, and the patterns are clear: UCAT adds value, above and beyond secondary school achievement, in predicting undergraduate performance.4
Of importance in this discussion is the awareness that, unlike some other aptitude and personality tests used in medical selection, UCAT data are made freely available to independent researchers who wish to ask questions about validity, use of the test, and so on. The UCAT consortium has a long history of using the findings from this research to enhance the test: https://www.ucat.ac.uk/about-us/published-research.
Moreover, it is inappropriate to extrapolate data across countries. The widening access landscape in Australia and the UK differs. For example, Coyle et al.5 compared widening participation to higher and medical education across the two countries. They found that discourses of social mobility and individual responsibility are still paramount in the UK. In contrast, the dominant discourse in Australia is social accountability in achieving equity and workforce diversity. The target groups are different: Australia has major inequities between Aboriginal and Torres Strait Islanders and other Australians, whereas the UK’s inequities are based mostly on social class issues. So too are practices – for example, Australia uses a quota system to ensure representation of students from remote and rural, and indigenous backgrounds in medical school. The UK takes a more meritocratic approach.
Our final point is that we need to stand back and stop focusing on which tool is ‘best’ for widening access. No one selection tool is going to provide the magic bullet in respect of addressing societal ills. Medical school selection is highly contextual, complex and politicised.6 We urge medical schools to shift from their predominant reductionist views of selection (the ‘best’ tool(s)) and instead explicitly acknowledge medical school selection in a way that respects complexity and uses disruption productively. Only by doing so can we create approaches to selection that are fit for purpose, fair and future-focused.
Jennifer Cleland1, Kathrine Gibson Smith2
1Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore
2Institute for Education in Medical and Dental Sciences, University of Aberdeen
Email: jennifer.cleland@ntu.edu.sg, kathrine.gibson.smith@abdn.ac.uk
doi: 10.4997/JRCPE.2021.227
References
1 Smith KG, Cleland J. Drastic times need drastic measures: COVID-19 and widening access to medicine. J R Coll Physicians Edinb 2020; 50: 431–435.
2 Griffin B, Horton GL, Lampe L et al. The change from UMAT to UCAT for undergraduate medical school applicants: impact on selection outcomes. Med J Aust 2021; 214: 84–89.
3 Powis DA, Munro D, Bore MR. Is the UCAT appropriate for selecting undergraduate medical students? Med J Aust 2021; 214: 77–78.
4 McManus IC, Dewberry C, Nicholson S et al. The UKCAT-12 study: educational attainment, aptitude test performance, demographic and socio-economic contextual factors as predictors of first year outcome in a cross-sectional collaborative study of 12 UK medical schools. BMC Med 2013; 11: 244. doi: 10.1186/1741-7015-11-244.
5 Coyle M, Sandover S, Poobalan A et al. Meritocratic and fair? The discourse of UK and Australia’s widening participation policies. Med Educ Dec 21 2020. https://onlinelibrary.wiley.com/doi/abs/10.1111/medu.14442.
6 Cleland JA, Patterson F, Hanson MD. Thinking of selection and widening access as complex and wicked problems. Med Educ 2018; 52: 1228–39.
What type of stroke do people on direct oral anticoagulants suffer?
Direct oral anticoagulants (DOAC) are increasingly used in patients with atrial fibrillation (AF) to prevent strokes. While they have been proven to be better than warfarin, patients can still suffer strokes despite taking a DOAC. We did an observational study on the nature of strokes people develop while on a DOAC as there is no data on this outside the clinical trials.
We identified patients admitted with a stroke while taking a DOAC during a three-year period (2018–2020) in a district general hospital. We gathered information on the nature of stroke and the type and dose of DOAC they’ve been taking.
During the three-year period, 1,238 patients were admitted with a stroke. 196 had AF, either at admission or identified during their hospital stay. In patients with AF on admission, 22 were on warfarin, 109 were on a DOAC and 49 were not on any anticoagulants.
Out of 109 patients taking a DOAC, 62 were taking a normal dose and 47 were taking a reduced dose as per recommendations. 56 took apixaban, 32 took edoxaban, 18 took rivaroxaban and 3 took dabigatran. 93 had an ischaemic stroke and 16 had a haemorrhagic stroke. Only one patient on edoxaban was non-compliant. 44 out of 56 patients on apixaban, 31 out of 32 patients on edoxaban, 15 out of 18 patients on rivaroxaban and all 3 on dabigatran had ischaemic strokes (see table below).
|
|
|
|
|
|
Edoxaban
|
30 mg od
|
0
|
19
|
|
Edoxaban
|
60 mg od
|
1
|
12
|
|
Apixaban
|
2.5 mg bd
|
3
|
18
|
|
Apixaban
|
5 mg bd
|
9
|
26
|
|
Rivaroxaban
|
15 mg od
|
3
|
4
|
|
Rivaroxaban
|
20 mg od
|
0
|
11
|
|
Dabigatran
|
150 mg bd
|
0
|
3
|
Apixaban and edoxaban were the most commonly used DOACs and dabigatran was the least commonly used. The majority of strokes (85%) that occurred while taking a DOAC were ischaemic in nature. Lower risk of haemorrhagic stroke (15%) on DOACs was consistent with results from all studies on stroke prevention in AF.1
Even though our numbers are too small for head-to-head comparison, in the apixaban group, the number of haemorrhagic strokes was higher with the higher dose. In the rivaroxaban group there was no relation between the dose and the nature of stroke and there were only three on dabigatran and all had ischaemic stroke. Almost all patients on edoxaban (97%) had ischaemic strokes.
Currently the choice of a DOAC largely depends on local guidelines. A meta-analysis of all DOACs found that apixaban 5 mg twice a day was the most effective drug for all outcomes compared with warfarin.1 In the clinical trial on edoxaban versus warfarin, lower-dose edoxaban was inferior to warfarin and its overall benefit was mainly due to a reduction in haemorrhagic strokes.2
One should use a DOAC that would be most effective, and the justification for its use to reduce the risk of haemorrhagic strokes shouldn’t be offset by the disproportionate increase in ischaemic strokes that seems to be the case for edoxaban. Since it is extremely unlikely that there would be a trial directly comparing all these drugs, data from a large cohort would be helpful and until then we recommend clinicians to use apixaban for stroke prevention in AF.
Helen Thomas1, Win Mar Soe2, Vedamurthy Adhiyaman3, Indrajit Chattopadhyay4
1Stroke Specialist Nurse, 2GPVTS Trainee, 3,4Consultant Geriatricians
Glan Clwyd Hospital, Rhyl, LL18 5UJ
Email: Vedamurthy.adhiyaman@wales.nhs.uk
doi: 10.4997/JRCPE.2021.228
References
1 López-López JA, Sterne JA, Thom HH et al. Oral anticoagulants for prevention of stroke in atrial fibrillation: systematic review, network meta-analysis, and cost effectiveness analysis. BMJ 2017; 359.
2 Giugliano RP, Ruff CT, Braunwald E et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med 2013; 369: 2093–104.
The end of the bedside clinical round?
In the current pandemic caused by COVID-19, a number of organisational changes have been presented in hospitals, with the aim of redistributing work spaces, economic flow and health personnel. Within these changes, patient-centred care times have been affected. Clinical practice guidelines on healthcare have recently been published in intensive care units such as Aziz et al.,1 where the authors mention that the pandemic can stun healthcare systems as the volume of critically ill patients increases, causing a severe shortage of trained critical care personnel. Also, they recommend minimising the number of personnel entering the rooms of positive COVID-19 patients.1 The following question arises: Because of the current pandemic, do we face the end of the clinical round as an academic activity and integration of knowledge for the healthcare of patients?
As described by Rimmelé et al.,2 excess mortality increases when healthcare organisations are overwhelmed with the number of patient admissions, and there is limited availability of professionals to care for them.2 However, it is important to consider strategies to optimise time without neglecting healthcare quality. A clear example of these strategies is the bedside clinical rounds, which promote patient-centred healthcare but also allow the discussion of clinical cases between health professionals and students, which leads to favourable results for the students, for the patients and for the health professionals who feel support in making decisions and have a space to clarify their doubts and those of the learner.3
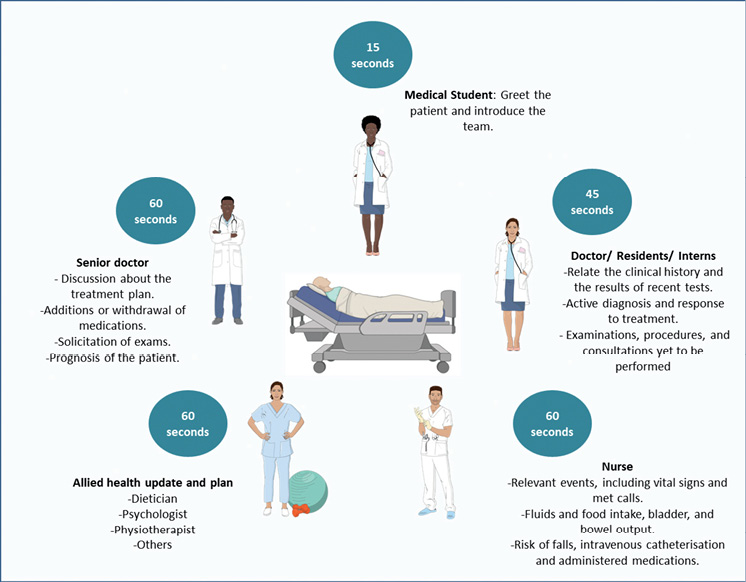
Understanding that, in the context of the actual pandemic, it can be challenging to carry out the clinical bedside rounds also is essential to highlight that the current clinical literature reports a possible solution; that solution is to establish structured interdisciplinary clinical bedside rounds (Figure 1) that optimise the visit time of patients, as established by Cao et al.,4 who demonstrated that a structured clinical bedside round has a shorter time than unstructured rounds, with significance of statistical data (P <0.01).4 Even this same study showed that there is a perception of improvement in patient management and clarity in the assignment of tasks for healthcare professionals (P <0.05).4 Other studies, such as that of Redley et al.,5 have also pointed out that the performance of structured interdisciplinary clinical bedside rounds has increased the participation of the healthcare professionals, improving the desired clinical behaviours and reducing the times of the clinical rounds, obtaining better outcomes for the patients.5
Figure 1 Proposal of a multidisciplinary structured clinical round in front of the patient (consisting of one senior doctor, one doctor or resident or intern, one medical student, one nursing professional and one allied professional). Distribution of time and activities among team members in a maximum time of four to five minutes, with the aim of rapidly and systematically evaluating the patient, making decisions based on the findings and putting passive learning into practice. Created with BioRender and Servier Medical Art.
We suggest to intensive healthcare professionals not to let these types of activities die: the structured clinical bedside rounds. These clinical rounds are intended to maintain academic activity and quality healthcare for patients. This valuable resource for our learning and timely treatment of individuals hospitalised in intensive care units cannot be missed, especially in times of COVID-19.
Yelson Picón-Jaimes1, Ivan Lozada-Martínez2, Luis Rafael Moscote-Salazar3, Tariq Janjua4
1Medical and Surgical Research Center, Centro Médico Medicien, Chile
2Medical and Surgical Research Center, University of Cartagena, Colombia
3Colombian Clinical Research Group in Neurocritical Care, University of Cartagena, Colombia
4Intensive Care, Regions Hospital, 640 Jackson St, Saint Paul, Minnesota, USA
Email: ilozadam@unicartagena.edu.co
doi: 10.4997/JRCPE.2021.229
References
1 Aziz S, Arabi YM, Alhazzani W et al. Managing ICU surge during the COVID-19 crisis: rapid guidelines. Intensive Care Med 2020; 46: 1303–25. doi: 10.1007/s00134-020-06092-5.
2 Rimmelé T, Pascal L, Polazzi S et al. Organizational aspects of care associated with mortality in critically ill COVID-19 patients. Intensive Care Med 2021; 47: 119–21. doi: 10.1007/s00134-020-06249-2.
3 Lichstein PR, Atkinson HH. Patient-centered bedside rounds and the clinical examination. Med Clin North Am 2018; 102: 509–19. doi: 10.1016/j.mcna.2017.12.012.
4 Cao V, Tan LD, Horn F et al. Patient-centered structured interdisciplinary bedside rounds in the medical ICU. Crit Care Med 2018; 46: 85–92. doi: 10.1097/CCM.0000000000002807.
5 Redley B, Campbell D, Stockman K et al. Mixed methods quality evaluation of structured interprofessional medical ward rounds. Intern Med J 2020; 50: 222–31. doi: 10.1111/imj.14330.
Putting spin on the great gamble
Gambling is a risky game of chance. The ‘gamble’ in medical career decision-making is in picking a job that will be a personal winner. Croghan and Baker’s paper in this journal, ‘The great gamble? A mixed methods study of factors influencing medical students’ specialty choice’,1 concluded that many factors influence career decision-making, including role models, exposure to specialties and perceived work–life balance.
These influencing factors are well known and, unfortunately, the use of a single small group discussion and a locally developed questionnaire inherently limited the possibility of generating new knowledge. Yet recent research looking at equivalent groups in the UK and Australia2,3 has progressed understanding of medical career decision-making by moving from the use of unvalidated if familiar questionnaire surveys to tools that force respondents to prioritise what is most important, and to examine how individuals ‘trade off’ different characteristics of a possible training post.
This is an important development: descriptive surveys can identify preferences but are only the start of knowledge-building. Identifying the relative strength, or value, of career preferences adds functionality by highlighting what are the most important push and pull factors for early-career doctors.
One tool for doing this is a discrete choice experiment (DCE). Based on consumer theory and used widely in health policy and planning,4 DCEs draw on earlier literature but are also underpinned by qualitative research, pre-piloting, piloting and statistical testing.5 This careful planning results in a robust quantitative tool that forces individuals to state their preference over hypothetical alternatives, in this case training posts (see Table 1 for an example DCE question).
Table 1 An example discrete choice experiment (DCE) question, from a national study of UK foundation year doctors, career decision-making push and pull factors1
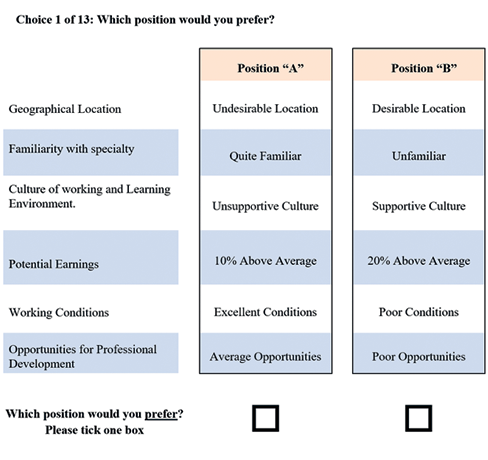
Each alternative is described by several characteristics (e.g. location, nature of the specialty), the levels of which vary over alternatives (e.g. high or low patient contact). This bundling together of characteristics mimics real life, where a product (e.g. car), a service (e.g. internet provider) or in this case a training position brings a set of intertwined characteristics, within which individuals must trade off the pros and cons (e.g. cost versus internet speed). For example, is location more important than specialty, or is salary less important than prestige?
Certain characteristics cannot be changed (e.g. geographical location, nationally set pay), but knowing what is valued by trainees can help healthcare employers and those in charge of medical training know what and by how much something else can be altered (e.g. working conditions, wellbeing resources, rotas). This in turn can compensate for the characteristic that cannot be influenced.6 And so, the game has two players – the trainee placing their employment bet and the employer seeking to attract and retain trainees.
It is essential to move from simple surveys to tools that identify the relative importance of various factors to doctors considering their options for postgraduate medical training. Only by doing so can we gather the intelligence needed to address what really matters to tomorrow’s doctors, their employers and the patients who need their services. Setting the odds right ensures positive gains for all parties.
Jennifer Cleland1, Peter Johnston2
1Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore
2Centre for Healthcare Education Research and Innovation (CHERI), School of Medicine, Medical Sciences and Nutrition, University of Aberdeen, UK
Email: jennifer.cleland@ntu.edu.sg
doi: 10.4997/JRCPE.2021.230
References
1 Croghan SM, Baker T. The great gamble? A mixed-methods study of factors influencing medical students in specialty choice. J R Coll Physicians Edinb 2020; 50: 422–430.
2 Scanlan GM, Cleland J, Johnston P et al. What factors are critical to attracting NHS foundation doctors into specialty or core training? A discrete choice experiment. BMJ Open 2018; 8: e019911. doi: 10.1136/bmjopen-2017-019911
3 Sivey P, Scott A, Witt J et al. Junior doctors’ preferences for specialty choice. J Health Econ 2012; 31:813–23.
4 Mandeville KL, Lagarde M, Hanson K. The use of discrete choice experiments to inform health workforce policy: a systematic review. BMC Health Serv Res 2014; 14: 367.
5 Kløjgaard M, Bech M, Søgaard R. Designing a stated choice experiment: the value of a qualitative process. J Choice Model 2012; 5: 1–18.
6 Cleland J, Porteous T, Skåtun D. What can discrete choice experiments do for you? Med Educ 2018; 52: 1113–1124.
Bridging the culture gap: it is time to address the cultural differences for the newly appointed overseas doctors in the NHS
Although there has been an increasing effort to support overseas doctors, the need to address the cultural gap seems to be overlooked. The current integration methods are based on a number of clinical tests followed by standard trust induction programmes, which are usually not tailored towards overseas doctors’ needs. One example of a supporting activity is the ‘Welcome to UK Practice’ run by the General Medical Council (GMC) consisting of a one-day session with various scenarios and ethical dilemmas.1 It is a gentle start for someone new in the NHS, albeit not enough to cover all that is needed for the long haul.
Integration does not happen straight away, and it is often a stressful transition for overseas doctors in the very first part of their journey in the NHS. These doctors gain their medical qualification from over 160 countries worldwide2 and each of these nations has its own unique culture and medical health regulations, which are often very different from those of the UK. Inherently, a number of challenges can arise consequent to these dissimilarities.3
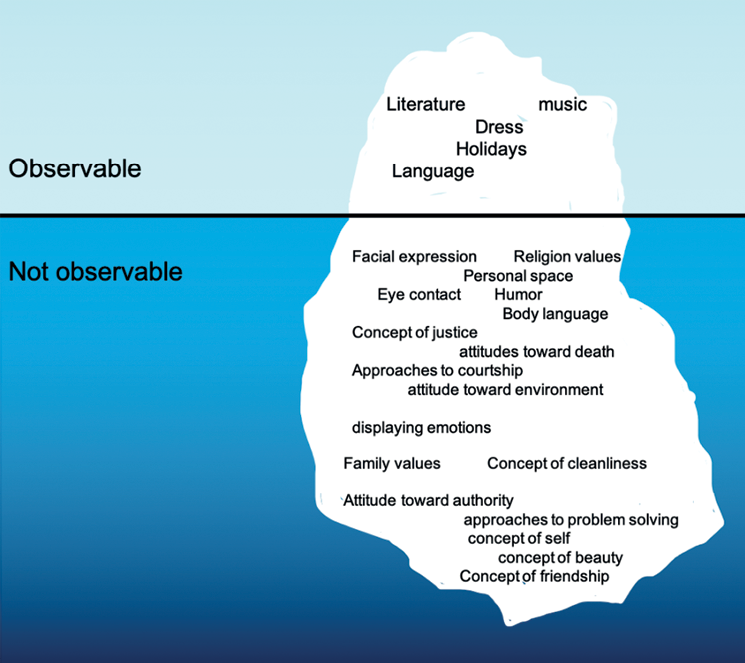
Culture is a complex social phenomenon and often referred to as ‘the unwritten rules of the social game’.4 An analogy to culture is the concept of the ‘cultural iceberg’, as proposed by Edward Hall in 1976.5 He stated that some aspects of a culture are visible, but the larger portion is hidden deep beneath the surface (Figure 1). A newly arrived foreign doctor may interact with cultural components like language, food, clothing and music. However, they are only interacting with the tip of the iceberg, as there are deeper elements that are often intangible and take longer to be perceived. An example of this is the subtlety of body language, which has different meanings in different cultures and can be easily misinterpreted.
Figure 1 Analogy to the concept of cultural complexity is the cultural iceberg. Some elements of culture are observable to a new overseas doctor, but the majority of cultural elements are not observable and hidden beneath the surface.
Another useful concept in this area is Geert Hofstede’s theory, which offers a new approach in understanding a national culture by giving it high or low scores in six main domains4 (Table 1). An overseas doctor coming from a high collectivist society, for example, may be perceived as a poor team player or less assertive when working in a high individualistic country like the UK.6 Thus, the iceberg concept and Hofstede’s theory can both be used as tools to aid understanding of the existing distinct cultural characteristics and their implications.
Table 1 Cultural dimensions of a nation as proposed by Geert Hofstede
|
|
High: hierarchical order, unequal power distribution accepted (e.g. China)
|
Low: equal distribution of power
(e.g. Germany, Great Britain)
|
|
|
Individualism: focus on individual needs and preferences (e.g. USA, Australia)
|
Collectivism: focus on whole group’s needs and goals (e.g. South Korea, China)
|
|
|
Masculine societies focus on material rewards for success, heroism, assertiveness, achievement-oriented
(e.g. Japan, China)
|
Feminine societies prefer quality of life, modesty, cooperation, care-oriented
(e.g. Norway, Sweden)
|
|
|
High: rigid behaviour and belief codes
(e.g. Greece, Japan)
|
Low: practice more important than principles, more tolerant to different opinions (e.g. Denmark, Sweden)
|
|
|
Long: open to new forms of education, pragmatic, perseverant (e.g. South Korea, Taiwan)
|
Short: prefer to maintain traditions and norms (e.g. Pakistan)
|
|
|
Indulgence: encourages gratification
(e.g. Latin America)
|
Restraint: strict social norms, suppresses gratification (e.g. East Asia)
|
These differences seem to be too vast to be tackled, but they are too important to ignore. We believe that a long-term, systematic ‘cultural integration’ can complement standard hospital induction programmes. The first step in bridging the cultural gap is to increase awareness among overseas doctors that such differences and challenges are inevitable, and that this information should be accessible on a single online resource hub. Equally, NHS staff should be educated about the rich cultural diversity of the NHS to create a working practice that recognises and respects cultural differences. Finally, on a par with most academic institutions, NHS trusts can adopt a ‘buddy scheme’ or ‘cultural ambassador’ for newly arrived overseas doctors, in order to help them settle within the local community. We believe these measures would allow overseas doctors to be better prepared within the NHS, permitting them to have not only greater cultural integration, but also an improved work environment, thus providing better care for patients.
Anna Zonato1, Mustafa Jalal2,3
1Accident and Emergency Department, Norfolk and Norwich University Hospitals, Norwich, UK
2Department of Infection, Immunology and Cardiovascular Diseases, University of Sheffield, Sheffield, UK
3Academic Department of Gastroenterology, Sheffield Teaching Hospitals, Sheffield, UK
Email: annazonato@gmail.com
doi: 10.4997/JRCPE.2021.231
References
1 GMC. Welcome to UK practice: information for doctors. https://www.gmc-uk.org/about/what-we-do-and-why/learning-and-support/wor... (accessed 26/2/21).
2 GMC. Registered doctors by country of primary medical qualification. https://data.gmc-uk.org/gmcdata/home/#/reports/The%20Register/World%20ma... (accessed 26/2/21).
3 Slowther A, Lewando Hundt GA, Purkis J et al. Experiences of non-UK-qualified doctors working within the UK regulatory framework: a qualitative study. J R Soc Med. 2012; 105: 157–65. doi:10.1258/jrsm.2011.110256.
4 Hofstede G. What is culture? https://geerthofstede.com/culture-geert-hofstede-gert-jan-hofstede/defin... (accessed 1/3/21).
5 Hall E. Beyond Culture. New York: Bantam Doubleday Dell Publishing Group; 1976.
6 Morrow G, Rothwell C, Burford B et al. Cultural dimensions in the transition of overseas medical graduates to the UK workplace. Med Teach 2013; 35: e1537–45. doi:10.3109/0142159X.2013.802298.
Snakebites – prevention is better than cure
I would like to thank the JRCPE for the recent editorial by Bawaskar, Bawaskar and Bawaskar on the global burden of snakebite envenoming,1 and the related clinical paper on Hypnale coagulopathy.2 As a public and global health student, it is encouraging to see a focus on this important yet long-neglected issue,3 which disproportionately affects poorer, rural communities.4
I write to draw readers’ attention to the related article in BBC Future, since published. This is a very readable and well-researched piece on snakebite with links for further reading and explores snakebite prevention (such as mosquito nets to avoid bites from the common krait, a leading cause of snakebite envenoming in India), diagnosis (such as thermal imaging to identify venom-induced inflammation) and treatment (antivenom and novel treatments, such as the potential of DMPS against saw-scaled viper venom).5
In addition to the use of mosquito nets, the BBC Future article provides another simple way to prevent snakebite: rubber boots.5 Importantly, the article also highlights the need to engage with communities, and avoid simply handing out rubber boots: similar schemes in Africa have failed because villagers sold off the valuable rubber or found the boots uncomfortable and stopped using them.5 Indeed, one of the four strategic aims of the World Health Organization’s snakebite envenoming prevention and control strategy is to ‘empower and engage communities’.4 An exemplar of community engagement and empowerment is SHE-India (www.she-india.org), which orchestrates low-resource, community-based actions, including educational posters and videos in multiple languages, first aid training and partnership with village leaders and influencers.6 Their awareness-raising will most likely have prevented countless snakebites from occurring, saving many lives and limbs, although SHE-India recognise the need for a sustained, funded study over an extended period to properly evaluate their work’s impact.6
Meanwhile, physicians have an important role in ensuring safe and effective treatment to improve outcomes for snakebite victims and save lives.4 Healthcare professionals and public health practitioners should work together to further raise awareness of this neglected, devastating disease, and to engage and empower those at risk to stop snakebites occurring in the first place. Prevention is better than cure.
Conflicts of interest
CJG works for Scottish Health Action on Alcohol Problems (SHAAP), based at the Royal College of Physicians of Edinburgh (RCPE).
Christopher J Graham1,2
1Master of Public Health (MPH) Student, Faculty of Biology, Medicine and Health, University of Manchester, Manchester, M13 9PL, UK
2Research & Projects Officer, Scottish Health Action on Alcohol Problems (SHAAP), Royal College of Physicians of Edinburgh (RCPE), 12 Queen Street, Edinburgh, EH2 1JQ, UK
Email: c.graham@rcpe.ac.uk
doi: 10.4997/JRCPE.2021.232
References
1 Bawaskar HS, Bawaskar PH, Bawaskar PH. The global burden of snake bite envenoming. J R Coll Physicians Edinb 2021; 51:7–8. doi: 10.4997/JRCPE.2021.102.
2 Naik BS. Hypnale coagulopathy: snake envenomation of a different kind. J R Coll Physicians Edinb 2021; 51: 31–36. doi: 10.4997/JRCPE.2021.108.
3 Snakebite-emerging from the shadows of neglect. The Lancet 2019; 393: 2175. doi: 10.1016/S0140-6736(19)31232-2.
4 World Health Organization. Snakebite envenoming: a strategy for prevention and control. Geneva: World Health Organization; 2019. https://www.who.int/snakebites/resources/9789241515641/en.
5 The global fight against snake bites. BBC Future. 2021 April 14. https://www.bbc.com/future/article/20210413-how-rubber-boots-can-save-pe....
6 Kadam P, Ainsworth S, Sirur FM et al. Approaches for implementing society-led community interventions to mitigate snakebite envenoming burden: the SHE-India experience. PLoS Negl Trop Dis 2021; 15: e0009078. doi: 10.1371/journal.pntd.0009078.