Introduction
‘We are all in this together.’ This sentiment has become a constant refrain since the COVID-19 pandemic started to affect the world, articulated by many people with privileged communication platforms – including politicians, supermarket brands, and even the celebrity Madonna.1 Of course this is true – the health of your neighbours affects your health. However, as has become increasingly clear over the course of the pandemic, we are not all equally affected. The pandemic has provided an unprecedented opportunity for some with greater social privilege to save money from commuting, learn the skills of making sourdough or, at the extreme, accrue more than US $100 billion as a result of increases in home shopping – in the case of Jeff Bezos, the founder and chief executive of Amazon.2 For many others, however, the pandemic has affected livelihoods and health in unprecedented ways.
While the proximal cause of the COVID-19 crisis is the emergence of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), its consequences and origins are multi-faceted. The novel virus combines high infectivity with severe disease, in contrast to more established infections. Evidence is growing for long-term physical and mental health sequelae of infection – ‘long COVID’.3,4 The high burden of disease threatens to overwhelm the health systems in many countries, including the UK. Uncontrolled infection leading to staff absence also threatened other essential services. In the absence of effective control of infection rates, lockdown measures have been repeatedly required in the UK. However, these measures can result in adverse health consequences – for example, through reduced delivery of effective healthcare for non-COVID conditions, financial losses, and missed educational opportunities.5The severe social and economic effects of both uncontrolled infection and lockdown measures during the pandemic heralds a societal disruption which will have myriad and long-lasting consequences.
Understanding the severity of the pandemic’s impact, particularly in the UK, requires an appreciation of the pre-pandemic context (Figure 1). Before the pandemic, health trends within the UK were already weakening. Life expectancy had been consistently improving since the Second World War, but had stalled since around 2010.6,7 Importantly, this fall cannot be attributed to a natural limit for life expectancy, since many other countries have continued to experience improvements, notably Japan – which is amongst the world’s best performers. While the exact causes are debated, it has been argued that austerity policies (including a broad range of cuts in public sector services, notably healthcare, social care, welfare benefits and education) made a major contribution.7 Those cuts have therefore meant that the UK’s National Health Service (NHS), as well as other services targeting the social determinants of health, were stretched even before the pandemic. Again, not all population subgroups appear to have suffered equally. Increases in infant mortality in England from 2014 to 2017, for example, affected deprived areas most, with rising child poverty accounting for about one-third of this increase.8Other major societal challenges before the pandemic, notably the climate emergency and Brexit, posed similar threats to population health.
Figure 1 The tracking of inequalities from pre-pandemic to post-pandemic
Socioeconomic inequalities are crucial in understanding the differential impacts of the pandemic. Sir Michael Marmot has shown how the pandemic has affected socioeconomic inequalities in health.9 However, socioeconomic position provides just one lens through which to study the pandemic. A diverse range of other characteristics also warrant consideration. Alongside the Black Lives Matter movement, the pandemic has drawn attention to the importance of ethnicity within our society.10 Any assessment of the differential impact of the pandemic on population subgroups must also consider gender and age. In this paper, we therefore aim to provide a broad overview of the ways diverse population subgroups have been affected by the COVID-19 pandemic in the UK, with a focus on ethnicity, gender and age. We plan to explore other important social characteristics like disability and occupation in due course.
Ethnic minorities
Since early in the pandemic, ethnic minorities have been experiencing disproportionate harms due to COVID-19.11-13In contrast to socioeconomic inequalities in health, where the most disadvantaged consistently demonstrate poorer outcomes, health outcomes are often not worse among ethnic minorities in the UK. Before the pandemic, all-cause mortality rates were lower in several ethnic minority groups than in the White British majority in both England and Scotland.14,15 Despite increased public awareness of issues of race and ethnicity, understanding of ethnic inequalities in health has been hampered by confusion around what ethnicity is – with an erroneous tendency to equate it to genetics – and a misunderstanding of the role of structural racism.16
Policy discussions and public debates during the pandemic within the UK have often focused on ‘Black, Asian and Minority Ethnic (BAME)’ groups. Along with others,17 we prefer to avoid this term for several reasons, including the conflation of diverse ethnic groups, selecting specific ethnic groups over others, and the well-established dislike of the term within ethnic minority communities. In the UK, the term ‘race’ has typically been used to refer to racial groups which were historically and incorrectly defined on the basis of perceived biological differences related to skin colour and other physical features.18 However, since this classification underpins discrimination experienced by different racial groups, its use for studying experiences of racism is important. In contrast, the term ‘ethnicity’ has a broader meaning, identifying groups of individuals based on shared cultural and social characteristics, instead of relying on physical attributes.19 It is a complex concept which includes country of birth, language, religion, culture and physical appearance – characteristics influenced by where an individual lives, their ancestry and, to a limited extent, their genetic background.20 White ethnic minority groups exist and can experience health inequalities across diverse health outcomes, including Eastern and Central European migrants to the UK and the gypsy and traveller community.
But why have ethnic minority communities experienced greater harm from COVID-19? This could arise from differential infection rates, differential consequences of infection or a combination of the two.21 While the evidence is rapidly evolving, current research suggests greater risk of infection is likely to play the major role: large ethnic differences in serological evidence of prior infection emerged within the representative Office for National Statistics (ONS) survey.22 However, differences in healthcare, as a consequence of either slower access or poorer quality of care, may also contribute. While UK evidence related to inequitable healthcare for COVID-19 remains limited, pre-pandemic research demonstrated such inequalities.23
The importance of structural racism has been central in the debate about drivers of ethnic inequalities. While individual experiences of discrimination due to someone else’s actions (interpersonal racism) are associated with poorer health,24 structural racism instead highlights how social mechanisms can result in embedded and persistent disadvantage.25 Structural racism includes the social forces which shape society, its institutions and people’s experiences, and results in ethnic minorities experiencing socioeconomic disadvantage.26 For example, these forces may manifest in poorer quality housing and less secure employment (Figure 2). Public Health England and others rightly concluded that structural racism plays a central role in driving ethnic inequalities in COVID-19.27 However, there is doubt whether the UK Government understands the role of structural racism in ethnic inequalities: one government medical advisor argued that ’structural racism is not a reasonable explanation’, instead suggesting that factors like jobs and housing – mechanisms through which structural racism operates – may be more important,28 a view also articulated by the equalities minister, Kemi Badenoch.29
Figure 2 Mechanisms underpinning ethnic inequalities
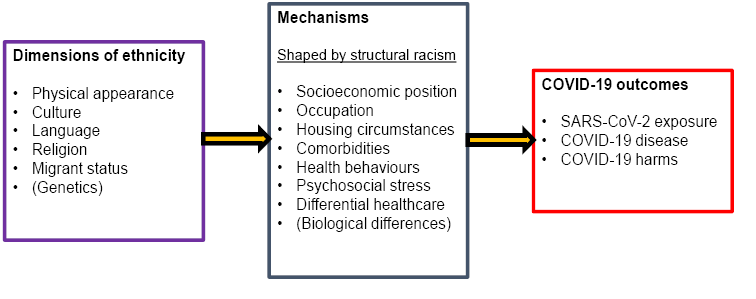
As the specific mechanisms driving ethnic inequalities in COVID-19 appear largely social (Figure 2), the importance of different mechanisms is likely to vary between settings and over time, and may lead to differing patterns of ethnic inequalities across different waves of the pandemic. In the UK, for example, Pakistani and Bangladeshi groups demonstrated disproportionate relative risks of death in the second wave compared with the first.30 After linking census and mortality records for England and Wales, accounting for differences in geographical and demographic factors weakens the relationship between ethnicity and COVID-19 deaths, but marked inequalities remain.31
Occupational differences are likely to be important, with ethnic minorities over-represented in some high-risk occupations, notably healthcare workers. Evidence also suggests that ethnic minority workers faced greater risks than the majority population within the same occupations – and greater difficulty in accessing personal and protective equipment.32,33 Insecure employment conditions like ‘zero hours’ contracts can render people unable to isolate themselves owing to financial barriers arising from lack of sick pay, leading individuals to delay seeking tests and accessing healthcare. Such insecure employment tends to be more common among some ethnic minorities.34 Differences in broader socioeconomic circumstances are also likely to play a role, with the most affluent in society better able to protect themselves from viral exposure – for example, by accessing goods and services online or using private transport. Housing circumstances are of particular importance in COVID-19, with smaller housing and lack of garden space making isolation and safer contact with family and friends more difficult. Some ethnic minorities are more likely to live in overcrowded accommodation, increasing transmissibility within the home; or in multi-generational households, where there is a risk of transmission from younger to older generations at greater risk of severe disease, because young people attend work or education.
Research investigating the contribution of biological and clinical factors has generally found that these do not greatly affect ethnic inequalities in COVID-19, as social factors are much more important.11,35 Studies identifying elevated risk of mortality in ethnic minorities have largely been based on administrative datasets with limited recording of social variables and thus been unable to fully investigate the potential mediating roles of social factors. Ethnicity does not have a strong genetic component, which is unsurprising given the longstanding migration of human populations throughout history. While genetic differences across ethnic groups have been sought and specific haplotypes identified that predict severe COVID-19, these have been found to play a very small role.36 Furthermore, adverse outcomes across diverse ethnic minorities indicates that genetic differences are unlikely to be important. Research into the impact of pre-pandemic health and clinical risk factors also indicates that they play a relatively small role.11,12 This is perhaps unsurprising, given that several ethnic minorities tended to have had better health before the pandemic – often related to health behaviours including lower levels of smoking and alcohol consumption. Obesity, however, is an important exception, with higher levels of obesity in some ethnic groups and potentially disproportionate COVID-19 harm arising from a similar body mass index.37
While most research to date within the UK has focused specifically on ethnicity, migration status is important and under studied. In general, migrants have relatively good health (referred to as the ‘healthy migrant’ effect) since people who are able to relocate their lives are typically a healthy subgroup of their population of origin.38 However, migrants may be disproportionately affected by the pandemic – particularly undocumented migrants (who lack paperwork for residence), refugees (who have legal entitlement to reside in a new country due to a well-founded fear of persecution) and asylum seekers (who are applying for refugee status)39– as suggested by a recent systematic review.40 The limited support from the UK Government – for example under the ‘no recourse to public funds’ condition of residency – may particularly affect these groups during periods of lockdown. While restrictions on entitlement to free healthcare for migrants have been waived for COVID-19 in England, confusion about such exemptions amongst both staff and patients threatens access to healthcare. Ensuring healthcare is available to all who need it remains crucial during the pandemic, especially to achieve control of infection rates.
While development of effective vaccines and delivery to high-risk groups has proceeded rapidly, willingness to take up the vaccine varies substantially by ethnicity. A large, representative study of UK adults indicated that Black or Black British people are much more vaccine hesitant (OR 13.5, 95% CI 7.6 to 24.2) than the White British majority.41Emerging evidence on vaccine uptake using linked administrative data in England echoes these findings.42 Addressing vaccine hesitancy in ethnic minority groups is crucial to prevent exacerbation of ethnic differentials in infection rates and outcomes. Adverse consequences of the pandemic and lockdown responses may also be differentially disadvantaging some ethnic minorities. For example, during the first UK lockdown, mental health among Asian ethnic groups deteriorated to a greater extent than in the White British group.43 Efforts to reduce vaccine-generated inequalities exacerbating existing ethnic inequalities are urgently required.
Gender
COVID-19 is more severe in men than women, with men at higher risk of both admission to intensive therapy unit (ITU) and death.44 However, the Office of National Statistics seroprevalence survey did not show a sex differential in positive serology, with evidence of similar levels of previous infection in both sexes.22 This sex differential in deaths therefore seems to relate mainly to poorer prognosis among men following infection – the virulence of which varies across the life course – rather than greater risk of contracting the infection.45 While the reasons underpinning this differential are not fully understood, it seems likely that a mixture of behavioural risk factors, occupational risks and genetic differences contribute. As an example of the role of behaviour, smoking has been established as a risk factor for severe COVID-19, and men in the UK have higher smoking rates than women, both currently and historically. Sex differences in risk factors may partially explain the gendered patterns of severe disease and mortality, alongside sex differences in health-seeking behaviours, such as choosing to access healthcare. The role of occupation needs to be further explored. Women might have been at greater risk of contracting COVID-19 and developing severe infection given the higher proportion of women working in high-risk frontline health and social care roles; however, this is not reflected in the data. One group of women who do appear vulnerable to COVID-19 are pregnant women, who are more likely to need intensive care treatment than women who are not pregnant.46
While there is widespread appreciation of the impact of the pandemic on men’s risk of COVID-19, rapid changes to the social determinants of health may mean that indirect harms have a greater impact on women’s health. Indeed, before the pandemic, women’s mental health had been declining during austerity policies which had differentially affected them.47 During the pandemic, the increased burden of childcare, resulting from school closures and discouraging grandparents from providing informal childcare because of age-related COVID-19 risks, has predominantly affected women, reducing their ability to work effectively. For single-parent families, which are more often led by a female parent, the impact of this increased childcare is felt more acutely, alongside the social isolation caused by lockdown. So it is not surprising that women’s mental health in the UK has declined even further during the pandemic.43
The longer-term economic impacts of COVID-19 on women in the labour market are also expected to be greater than for men. Whilst the furlough scheme has protected income for many in the UK during the lockdown period, the likely economic consequences of the pandemic include further job losses, particularly as business adapts to the “new normal” of the post-pandemic world.48 Whilst unemployment and its adverse health consequences will affect both men and women, women may be disproportionately affected by job losses owing to the greater proportion of women employed in the most adversely affected sectors.49
The direct effects of COVID-19 in the transgender and gender-diverse populations have not been well captured; however inequities in healthcare access observed before the pandemic may have resulted in trans people being more hesitant to seek healthcare for COVID-19.50 The absence of data capturing gender identity in health records means any effect is challenging to quantify.51 Healthcare disruption during the pandemic has impaired access to medical and surgical gender-affirming interventions. Adverse mental health indicators, which are more commonly observed in the trans population, tend to improve following gender-affirming treatment.52 Therefore pandemic-related delays in intervention may amplify the existing disparities in mental health outcomes for trans people. Social factors, including loss of support networks or being restricted to unsafe home environments through lockdown, may also contribute to deteriorating mental health.
Age
Age is a key risk factor for nearly all health outcomes, with COVID-19 no exception. Increasing age is by far the strongest predictor of COVID-19 mortality, with the UK vaccination programme consequently prioritised mainly by age. The risks of COVID-19 to the elderly are further intensified by the adverse impacts of restricting social interaction face to face, thereby exacerbating loneliness and its effects on mental and physical health. While loneliness is more common in young people and those living alone in the UK,53 COVID-19 related restrictions may be particularly difficult for the elderly and people with fewer financial resources.54 Balancing infection risk against concern that people living in care homes may be unable to meet family and friends has been challenging – especially given the very high mortality risks associated with COVID-19 in this setting.55
Ultimately, the pandemic is likely to have effects across the life course. Although children typically experience less severe illness from COVID-19 compared with adults, they are not immune to severe disease and a small proportion will develop potentially fatal complications, including multisystem inflammatory syndrome.56 However, for most children, the long-term consequences of COVID-19 are of greater significance. Given the crucial role of the early years in reducing health inequalities, lost educational opportunities may exacerbate the pre-pandemic trend towards increasing socioeconomic inequalities in health.57 Evidence suggests that reduced social interactions may also impede childhood development,58 as may parental stress resulting from the pandemic. Children have also been disproportionately affected by increasing poverty, which is linked to adverse lifelong health consequences.59
Young adults are also at risk of adverse long-term effects from the pandemic. While university students have been widely discussed in the media, vocational education that is less amenable to distance learning has also been affected. Evidence from previous recessions suggests that difficulty entering the labour market can negatively affect employment and earning opportunities in short- and long-term – often referred to as the ‘scarring’ effect of economic crises. In addition to high unemployment-related risks to physical and mental health,60,61 young adults appear to be at particular risk of adverse long-term health consequences of economic crises.62 Delays to other important transitions, especially partnership formation and child rearing, may also have lasting consequences.
The future
The COVID-19 pandemic has caused unprecedented societal disruption, forcing us to rethink both our approach to healthcare and to broader society. The pandemic continues to affect individuals and society both through the direct effects of widespread infection, resulting in a large death toll and longstanding disability for many survivors, and through myriad indirect pathways. In the absence of a competent test, trace, isolate and support system, severe lockdown restrictions have been repeatedly necessary and thereby disrupted essential services, including healthcare for conditions other than COVID-19. The lack of effective control over the pandemic has also resulted in widespread and prolonged economic disruption, threatening livelihoods and risking future cuts to government expenditures on health-promoting services.
Analyses of the pandemic’s impacts across population subgroups demonstrates the need for improvements in data and monitoring. Collection and analysis of health data during the pandemic has helped to inform our response; however, health datasets still lack accurate ethnicity information. This is a critical issue given its importance to health, and the legal obligation for the NHS to monitor equity of delivery. Data on occupation and housing circumstances are also unavailable and could have provided valuable evidence for policy – for example, estimates of COVID-19 risks among teachers and other professions.
To date, the COVID-19 pandemic has affected different population subgroups in very different ways. This looks set to continue. Policy responses to the developing economic crisis will have marked impacts on future health, particularly for those with the least social resources. On one hand, the pandemic has highlighted the systemic racism that continues to operate throughout UK society, the precarious employment conditions of many essential workers, and the inadequacy of the social safety net provided by the welfare system. Policy responses to tackle these longstanding challenges could help drive improvements in population health and potentially reduce the burden on the healthcare system. On the other hand, a policy response based on austerity could worsen population health and widen health inequalities. Given that ethnic minorities, women and young people are more likely to have precarious work, and are at greater risk of job loss, the need to monitor how health and its social determinants evolve is paramount as we move out of the pandemic. Following the pandemic, the climate emergency will become ever more urgent, so responding to it will be the major public health challenge of this century. Thus it is essential to consider the needs of all population groups when responding to the challenge to ‘build back better’.
References
1 Sobande F. ‘We’re all in this together’: Commodified notions of connection, care and community in brand responses to COVID-19. European Journal of Cultural Studies 2020; 23: 1033-37.
2 Neate R. Ten billionaires reap $400bn boost to wealth during pandemic [Internet]. London: The Observer. 19 December 2020. [Accessed 7 February 2021]. Available from: https://www.theguardian.com/technology/2020/dec/19/ten-billionaires-reap...
3 Niedzwiedz CL, Benzeval M, Hainey K et al. Psychological distress among people with probable COVID-19 infection: analysis of the UK Household Longitudinal Study. medRxiv 2020; 2020.11.24.20237909.
4 del Rio C, Collins LF, Malani P. Long-term health consequences of COVID-19. JAMA 2020; 324: 1723-24.
5 Douglas M, Katikireddi SV, Taulbut M et al. Mitigating the wider health effects of covid-19 pandemic response. BMJ 2020; 369: m1557.
6 Fenton L, Minton J, Ramsay J et al. Recent adverse mortality trends in Scotland: comparison with other high-income countries. BMJ Open 2019; 9: e029936.
7 Hiam L, Dorling D, McKee M. Things fall apart: the British health crisis 2010–2020. Br Med Bull 2020; 133: 4-15.
8 Taylor-Robinson D, Lai ETC, Wickham S et al. Assessing the impact of rising child poverty on the unprecedented rise in infant mortality in England, 2000-2017: time trend analysis. BMJ Open 2019; 9: e029424.
9 Marmot M, Allen J. COVID-19: exposing and amplifying inequalities. J Epidemiol Community Health 2020; 74: 681-82.
10 Cerdeña JP, Plaisime MV, Tsai J. From race-based to race-conscious medicine: how anti-racist uprisings call us to act. The Lancet 2020; 396: 11252-8.
11 Niedzwiedz CL, O’Donnell CA, Jani BD et al. Ethnic and socioeconomic differences in SARS-CoV-2 infection: prospective cohort study using UK Biobank. BMC Medicine 2020; 18: 160.
12 Williamson EJ, Walker AJ, Bhaskaran K et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature 2020; 584: 430-36.
13 Sze S, Pan D, Nevill CR et al. Ethnicity and clinical outcomes in COVID-19: a systematic review and meta-analysis. EClinicalMedicine 2020; 29: 100630.
14 Public Health England. COVID-19: review of disparities in risks and outcomes [Internet]. London: Public Health England; 2 June 2020. [Accessed 7 February 2021]. Available from: https://www.gov.uk/government/publications/covid-19-review-of-disparitie....
15 Bhopal RS, Gruer L, Cezard G et al. Mortality, ethnicity, and country of birth on a national scale, 2001-2013: a retrospective cohort (Scottish Health and Ethnicity Linkage Study). PLoS Med 2018; 15: e1002515.
16 Yudell M, Roberts D, DeSalle R et al. Science and society: taking race out of human genetics. Science 2016; 351: 564-65.
17 Aspinall PJ. BAME (black, Asian and minority ethnic): the ‘new normal’ in collective terminology. J Epidemiol Community Health 2021; 75: 107.
18 Bhopal R. Is research into ethnicity and health racist, unsound, or important science? BMJ 1997; 314: 1751.
19 Bhopal RS. Migration, Ethnicity, Race, and Health in Multicultural Societies. Oxford: Oxford University Press; 2014.
20 Bhopal R. Glossary of terms relating to ethnicity and race: for reflection and debate. J Epidemiol Community Health 2004; 58: 441-45.
21 Katikireddi SV, Lal S, Carrol ED et al. The unequal impact of the COVID-19 crisis on minority ethnic groups: a framework for understanding and addressing inequalities. J Epidemiol Community Health 2021; in press.
22 Office for National Statistics. Coronavirus (COVID-19) Infection Survey: characteristics of people testing positive for COVID-19 in England, August 2020. London: ONS; 18 August 2020. [Accessed 7 February 2021]. Available from: https://ons.gov.uk/releases
23 Katikireddi SV, Cezard G, Bhopal RS et al. Assessment of health care, hospital admissions, and mortality by ethnicity: population-based cohort study of health-system performance in Scotland. The Lancet Public Health 2018; 3:e226-e36.
24 Priest N, Paradies Y, Trenerry B et al. A systematic review of studies examining the relationship between reported racism and health and wellbeing for children and young people. Soc Sci Med 2013; 95: 115-27.
25 Nazroo JY, Bhui KS, Rhodes J. Where next for understanding race/ethnic inequalities in severe mental illness? Structural, interpersonal and institutional racism. Sociol Health Illn 2020; 42: 262-76.
26 Gee GC, Ford CL. Structural racism and health inequities: old issues, new directions. Du Bois Review: social science research on race 2011; 8: 115.
27 Public Health England. Beyond the data: understanding the impact of COVID-19 on BAME groups [Internet]. London: Public Health England; June 2020 [Accessed 7 February 2021]. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploa...
28 BBC News. Ethnic minority Covid risk ‘not explained by racism’ [Internet]. London: BBC; 22 October 2020 [Accessed 7 February 2021]. Available from: https://www.bbc.co.uk/news/health-54634721
29 BBC News. Coronavirus: Minister Kemi Badenoch rejects ‘systemic injustice’ claims [Internet]. London: BBC; 4 June 2020 [Accessed 20 March 2021]. Available from: https://www.bbc.co.uk/news/uk-politics-52913539
30 Nafilyan V, Islam N, Mathur R et al. Ethnic differences in COVID-19 mortality during the first two waves of the coronavirus pandemic: a nationwide cohort study of 29 million adults in England. medRxiv 2021; 2021.02.03.21251004.
31 Ayoubkhani D, Nafilyan V, White C, et al. Ethnic-minority groups in England and Wales—factors associated with the size and timing of elevated COVID-19 mortality: a retrospective cohort study linking census and death records. Int J Epidemiol 2020; 49: 1951-62.
32 Nguyen LH, Drew DA, Graham MS et al. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. The Lancet Public Health 2020; 5:e475-83.
33 Mutambudzi M, Niedwiedz C, Macdonald EB et al. Occupation and risk of severe COVID-19: prospective cohort study of 120 075 UK Biobank participants. Occup Environ Med 2020; oemed-2020-106731.
34 Bowyer G, Henderson M. Race inequality in the workforce: exploring connections between work, ethnicity and mental health [Internet]. Dunfermline: Carnegie UK Trust; February 2020. [Accessed 7 February 2021). Available from: https://d1ssu070pg2v9i.cloudfront.net/pex/carnegie_uk_trust/2020/03/2716...
35 Nafilyan V, Islam N, Ayoubkhani D et al. Ethnicity, household composition and COVID-19 mortality: a national linked data study. J R Soc Med 2021.
36 Zeberg H, Pääbo S. The major genetic risk factor for severe COVID-19 is inherited from Neanderthals. Nature 2020; 587: 610-12.
37 Sattar N, Ho FK, Gill JMR et al. BMI and future risk for COVID-19 infection and death across sex, age and ethnicity: Preliminary findings from UK biobank. Diabetes & Metabolic Syndrome: Clinical Research & Reviews 2020; 14: 1149-51.
38 Aldridge RW, Nellums LB, Bartlett S et al. Global patterns of mortality in international migrants: a systematic review and meta-analysis. The Lancet 2018; 392: 2553-66.
39 Urquia ML, Gagnon AJ. Glossary: migration and health. J Epidemiol Community Health 2011.
40 Hintermeier M, Gencer H, Kajikhina K et al. SARS-CoV-2 among migrants and forcibly displaced populations: a rapid systematic review. medRxiv 2020; 2020.12.14.20248152.
41 Robertson E, Reeve KS, Niedzwiedz CL et al. Predictors of COVID-19 vaccine hesitancy in the UK Household Longitudinal Study. Brain Behav Immun 2021.
42 MacKenna B, Curtis HJ, Morton CE et al. Trends, regional variation, and clinical characteristics of COVID-19 vaccine recipients: a retrospective cohort study in 23.4 million patients using OpenSAFELY. medRxiv 2021; 2021.01.25.21250356.
43 Niedzwiedz CL, Green MJ, Benzeval M et al. Mental health and health behaviours before and during the initial phase of the COVID-19 lockdown: longitudinal analyses of the UK Household Longitudinal Study. J Epidemiol Community Health 2020; jech-2020-215060.
44 Peckham H, de Gruijter NM, Raine C et al. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nature Communications 2020; 11: 6317.
45 Bhopal SS, Bhopal R. Sex differential in COVID-19 mortality varies markedly by age. Lancet (London, England) 2020; 396: 532-33.
46 Allotey J, Stallings E, Bonet M et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ 2020; 370: m3320.
47 Thomson RM, Niedzwiedz CL, Katikireddi SV. Trends in gender and socioeconomic inequalities in mental health following the Great Recession and subsequent austerity policies: a repeat cross-sectional analysis of the Health Surveys for England. BMJ Open 2018; 8: e022924.
48 Costa Dias M, Joyce R, Postel-Vinay F et al. The challenges for labour market policy during the COVID-19 pandemic. Fiscal Studies 2020; 41: 371-82.
49 Alon TM, Doepke M, Olmstead-Rumsey J et al. The impact of COVID-19 on gender equality [Internet]. Cambridge: National Bureau of Economic Research; 2020. [Accessed 7 February 2021]. Available from: https://www.nber.org/system/files/working_papers/w26947/w26947.pdf
50 Winter S, Diamond M, Green J et al. Transgender people: health at the margins of society. The Lancet 2016; 388: 390-400.
51 Thomson RM, Katikireddi SV. Improving the health of trans people: the need for good data. The Lancet Public Health 2019; 4: e369-e70.
52 Bränström R, Pachankis JE. Reduction in mental health treatment utilization among transgender individuals after gender-affirming surgeries: a total population study. A J Psychiatry 2020; 177: 727-34.
53 Bu F, Steptoe A, Fancourt D. Who is lonely in lockdown? Cross-cohort analyses of predictors of loneliness before and during the COVID-19 pandemic. Public Health 2020; 186: 31-34.
54 Green MJ, Whitley E, Niedzwiedz CL et al. Social contact and inequalities in depressive symptoms and loneliness among older adults: a mediation analysis of the English Longitudinal Study of Ageing. SSM – Population Health 2021; 100726.
55 Salcher-Konrad M, Jhass A, Naci H et al. COVID-19 related mortality and spread of disease in long-term care: a living systematic review of emerging evidence. medRxiv 2020; 2020.06.09.20125237.
56 Swann OV, Holden KA, Turtle L et al. Clinical characteristics of children and young people admitted to hospital with covid-19 in United Kingdom: prospective multicentre observational cohort study. BMJ 2020; 370: m3249.
57 Marmot M. Health equity in England: the Marmot review 10 years on. BMJ 2020; 368.
58 Araújo LAd, Veloso CF, Souza MdC et al. The potential impact of the COVID-19 pandemic on child growth and development: a systematic review. J Pediatr (Rio J) 2020.
59 Cooper K, Stewart K. Does household income affect children’s outcomes? A systematic review of the evidence. Child Indicators Research 2020.
60 Roelfs DJ, Shor E, Davidson KW et al. Losing life and livelihood: a systematic review and meta-analysis of unemployment and all-cause mortality. Soc Sci Med 2011; 72: 840-54.
61 Milner A, Page A, Lamontagne AD. Cause and effect in studies on unemployment, mental health and suicide: a meta-analytic and conceptual review. Psychol Med 2014; 44: 909.
62 Strandh M, Winefield A, Nilsson K et al. Unemployment and mental health scarring during the life course. Eur J Public Health 2014; 24: 440-45.
