Introduction
Academic medicine encompasses doctors who combine a clinical career with teaching, research and health management.1 As part of the Modernising Medical Careers initiative, in 2005, Professor Sir Mark Walport identified that the pursuit of a clinical academic career was hindered by lack of a clear career structure, inflexibility and a shortage of posts.2 Concerns have been raised that recruitment into academic medicine has been inadequate. There are fears of a lost generation of young clinical academics,3 as numbers decline.4 We have previously published on this matter as we believe that the notion of ‘doctors as scholars’ has been a neglected competence within medical education.5 We have previously explored ways in which we can motivate medical students wishing to pursue clinical academia.6
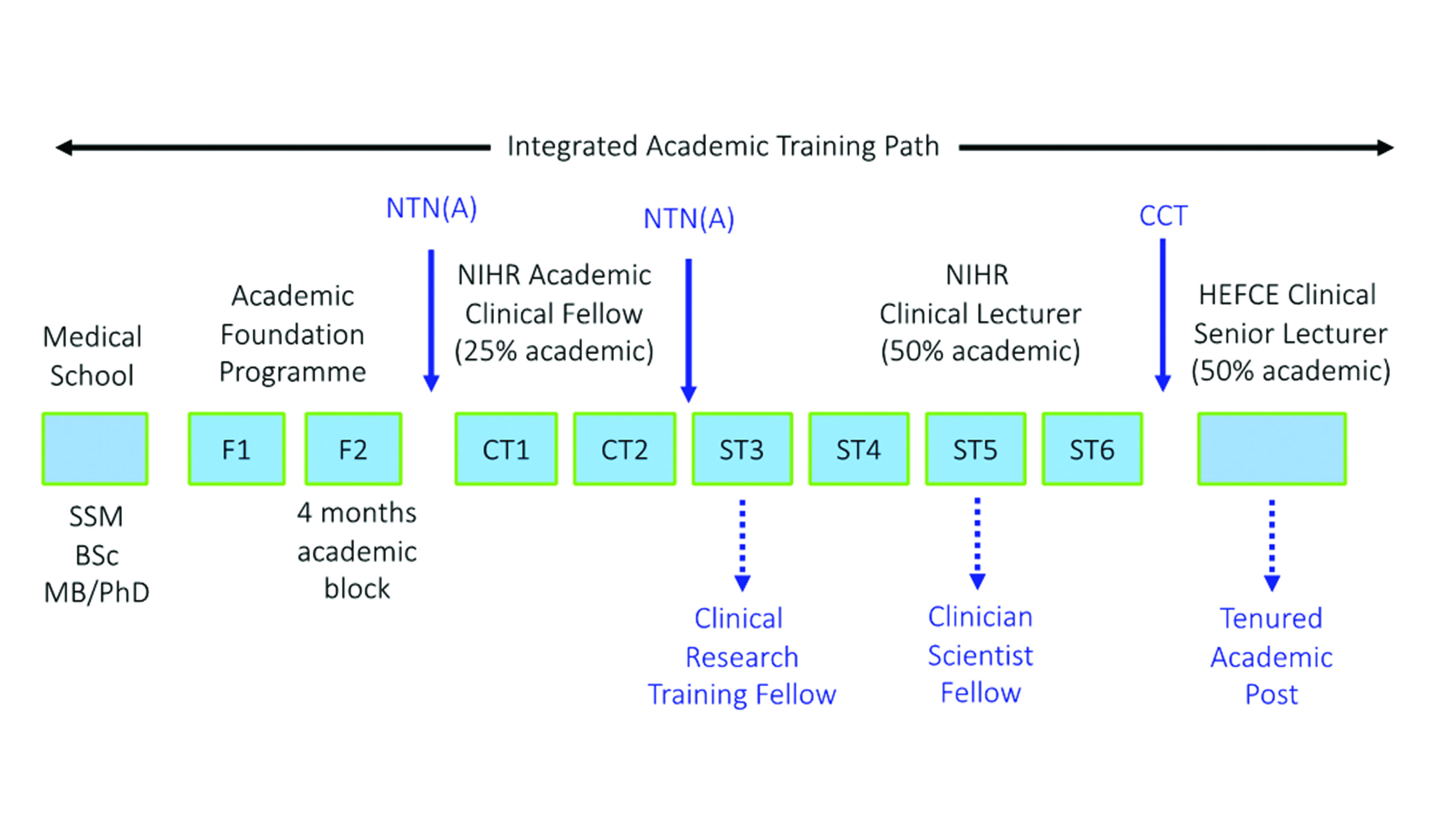
In order to combat this, a streamlined career structure was created, known as the Integrated Clinical Academic Pathway (Figure 1).2 The first step of this pathway is the academic sister to the foundation programme – the Academic Foundation Programme (AFP). The aim of the programme is to afford newly graduated doctors’ time within their 2-year training programme to explore a branch of academia of their interest. The most common structure for this is a ‘4-month block’ in the second year, giving junior doctors the opportunity to engage in research, teaching or management and even pursue further qualifications, such as diplomas.2,7–9 However, in deaneries such as in Scotland, not all posts have dedicated academic time within the second foundation year.9 In these programmes, clinical and academic training run parallel to one another.
Figure 1 The UK integrated clinical academic pathway. CCT: Certificate of Completion of Training; CT1/2: Core Training 1 and 2; F1/F2: Foundation Years 1 and 2; HEFCE: Higher Education Funding Council for England; NIHR: National Institute for Health Research; NTN(A): Academic National Training Number; SSM: student selected module; ST3-6: Specialist Training 3–6
Competition for the AFP posts has increased over recent years. The average competition ratio for applicants to AFP posts has increased from 1:3 in 2016 to 1:5 in 2018.10 While the number of applications have increased, the AFP only accounts for 5% of foundation posts.11 Despite this, students are often unaware of the process.6 Research conducted by Mashar et al.12 highlighted the ‘institutional disparity’ that can limit students from different medical schools from pursuing clinical academia. This results in prospective applicants often feeling unsure about how to proceed in pursuing a clinical academic career.
Webinars or web-based seminars are live lectures transmitted via the internet. A noted benefit of webinars is the fact they can reach a wider audience, without the restrictions of location.13 Attendees only require an internet connection and a device, minimising travel expenses and inconvenience to trainees.13 Live webinars allow for interaction, where attendees actively participate and can receive immediate feedback.13,14
The utility of webinars has been recognised by many of the Royal Colleges. They have been increasingly adopted for continuing medical education. For example, the Royal Colleges of Surgeons of England and Edinburgh hold regular webinars. These webinars provide accessible advice for members, covering topics from how to write a paper to the latest on less than full-time training. Additionally, an archive of past webinars is maintained for members to peruse at later dates.15,16 Despite the increased utilisation of webinar as a teaching medium, there are limited studies within the medical education literature assessing their efficacy.
Our goal was to hold a webinar to provide students with an outline of the UK integrated clinical academic pathway and encourage them to apply for the AFP. Therefore, we aimed to evaluate the usefulness and utility of webinars as a teaching platform and to further evaluate the role of webinars in facilitating students’ interest in academia. Utility and usefulness were assessed through participant’s self-rated knowledge, confidence and interest as this would highlight that webinars can achieve comparable results to similar ‘live-classroom teaching events’.
Methods
We organised a free webinar for UK medical students using an online platform. The webinar was designed and delivered by AK, a former academic foundation trainee. We provided a brief outline of an integrated clinical academic career, focusing on the first step of this pathway, the AFP. We discussed the application process, pros and cons of the programme and how it can be used as a springboard into academic medicine. Our aim was to motivate potential applicants and enhance student interest in academia. As this project was an evaluation of a teaching intervention, ethical approval was not required. No incentives were offered for completing the questionnaire, nor did it affect their attendance to the webinar and students were informed that the purpose of the questionnaire was for assessing the success of the webinar.
Attendees were invited to participate in a cross-sectional study with a pre- and post-webinar questionnaire. Our inclusion criteria was UK medical students who were registered to attend the webinar. The questionnaires were emailed out to attendees via the mailing list of registered attendees. We used Google Forms (Google, USA) as our online questionnaire platform, which stores data in a Google Sheets (Google, USA) encrypted database. Attendees were given 1 week prior to the webinar to complete the pre-webinar questionnaire and 1 week afterwards to complete the post-webinar questionnaire.
The pre-webinar questionnaire collected data on student demographics, their medical school and desired units of application. We also collected data on students’ beliefs about the use of webinars as educational tool and where students have previously accessed information about a clinical academic career (Table 1). Questions evaluating factors such as self-rated knowledge, confidence and interest about the AFP were designed with a Likert scale (1 = low, 5 = high) and used in both questionnaires (Tables 1 and 2).
Table 1 Pre-webinar questionnaire
Name | |
Email | |
Gender | |
Year of medical school | |
Are you an undergraduate or graduate entry-medic? | - Undergraduate Medicine
- Graduate Entry Medicine
|
Have you undertaken an additional degree? | - BSc
- BMedSci
- MSc
- MRes
- MD
- PhD
- Considering an intercalated degree
- I do not have an additional degree
|
What academic units of application are you considering applying to? | - East Anglia: Cambridge
- East Anglia: Norfolk and Norwich
- Essex, Bedfordshire, Hertfordshire
- East Midlands
- London
- Northern
- North West of England
- Oxford
- South West
- Wales
- West Midlands
- Yorkshire and Humber
|
How many webinars for medical education have you attended? | |
Have you previously attendee a webinar on clinical academic training and/or the academic foundation programme? | |
To what extent do you agree or disagree with the statement ‘webinars offer flexibility and convenience with for example, not having to spend time and money on travelling’? | Likert Scale 1–5: Strongly Disagree to Strongly Agree |
Would you prefer a face-to-face tutorial to a webinar? | - Face-to-face tutorial
- Webinar
- I do not mind
|
How easy has it been to find research opportunities within medical school? | Likert Scale 1–5: Extremely Difficult to Extremely Easy |
How interested are you in applying to the Academic Foundation Programme? | Likert Scale 1–5: Extremely Uninterested to Extremely Interested |
How knowledgeable do you feel about the AFP application process? | Likert Scale 1–5: Extremely Unknowledgeable to Extremely Knowledgeable |
How confident do you feel about the AFP application process? | Likert Scale 1–5: Very Doubtful to Very Confident |
To what extent has your university informed you about a career in clinical academia (the AFP and beyond?) | Likert Scale 1–5: Minimal Advice to Extensive Advice |
What other resources have you used to learn more about the AFP application process? | - Websites
- Published Journal Articles
- Books
- Courses (not organised by the university)
- University (Lectures, Careers Team)
- University Societies, e.g. academic medicine society, surgical society
- Friends and colleagues
- Nothing
|
Table 2 Post-webinar questionnaire
Name | |
Email Address | |
To what extent do you agree or disagree with the statement ‘this webinar was engaging and enjoyable?’ | Likert Scale 1–5: Strongly Disagree to Strongly Agree |
To what extent do you agree or disagree with the statement ‘the webinar taught me something which I consider valuable?’ | Likert Scale 1–5: Strongly Disagree to Strongly Agree |
How interested are you in applying to the AFP after this webinar? | Likert Scale 1–5: Extremely Uninterested to Extremely Interested |
How knowledgeable do you feel about the AFP application process after this webinar? | Likert Scale 1–5: Extremely Unknowledgeable to Extremely Knowledgeable |
On a scale of 1 to 5, how confident do you feel about the AFP application process after this webinar? | Likert Scale 1–5: Very Doubtful to Very Confident |
To what extent do you agree or disagree with the statement ‘my interest in the AFP has increased as a consequence of this webinar’ | Likert Scale 1–5: Strongly Disagree to Strongly Agree |
How easy did you find it to interact/submit questions? | Likert Scale 1–5: Extremely Difficult to Extremely Easy |
Are you more or less likely to ask questions in a webinar or live lecture? | - More Likely
- Equally likely
- Less likely
|
Are you more or less likely to participate in a future webinar based on this experience? | Likert Scale 1–5: Extremely Unlikely to Extremely Likely |
Any other feedback | |
The nonparametric Wilcoxon matched-pairs rank sum tests were performed to analyse the pre- and post-webinar measure of knowledge, interest and confidence in the AFP application process. Statistical analysis was calculated using R (version 3.4.0).
Results
A total of 199 students signed up for the webinar, from 21 different UK medical schools. The median age of participant was 22 (range: 20–29) years old. In total, 118 out of 199 (59.3% response rate) attendees filled out the pre-webinar questionnaire, while 64 out of 199 attendees (32.2% response rate) filled out the post-webinar questionnaire. The response rate of matched questionnaires was 45 out of 118 (38.1%).
The majority of attendees were undergraduate students, 91.5% (108), whereas 8.5% (10) were graduate-entry medical students. Predominantly students were in their final or penultimate year of study, 70.3% (83 out of 118). Furthermore, 77.1% (91) had an additional degree, with 49.2% (58) having a BSc, 10.2% (12) having an MSc, 9.3% (11) having a BMedSci, 8.5% (10) having an MRes and 3.4% (4) having a PhD.
A total of 38 (32.2%) attendees felt they had only received minimal advice and a further 33 (27.8%) felt that they had been given no advice regarding pursuit of a clinical academic career from their place of study. In terms of prior webinar attendance, 83.1% (98) had never attended a medical education webinar. Only 1.7% (2) had previously attended a webinar specific to clinical academic training.
A total of 32.2% (38) of attendees stated that they preferred webinars to face-to-face teaching. A preference for face-to-face teaching was stated by 14.4% (17), whereas 53.4% (63) asserted that they did ‘not mind’ between either teaching method. A total of 71.2% (84) strongly agreed and 20.3% (24) agreed that ‘webinars offer flexibility and convenience with, for example, not having to spend time and money on travelling’.
For participants that completed both questionnaires, the data demonstrated an increase in participants’ self-rated knowledge (median score: 3 [interquartile range (iQr): 2–3] vs 4 [iQr: 4–4], p < 0.0001, ci 2.000–2.000) and self-rated confidence [median score: 3 (iQr: 2–3) vs 3 (iQr: 2.75–4), p < 0.001, ci 2.000–2.000] of the AFP application process. There was no statistically significant difference in participant’s self-rated interest in pursuing an AFP [median score: 4 (iQr: 4–5) vs 5 (iQr: 4–5)].
For the post-webinar questionnaire, a total of 68.8% (44) were more likely to ask questions in a webinar than in a live lecture, with 29.7% (19) being equally likely to ask questions. A total of 82.8% (53) of participants in the post-webinar survey agreed or strongly agreed that ‘the webinar had taught them something which they considered valuable’. A further 82.8% (53) of participants stated they were more likely to participate in a future webinar based on this experience.
Discussion
To our knowledge, this is the first use of a live broadcast, webinar-based education programme to inform students about the UK clinical academic training pathway. In the past, our group has explored how a live teaching course may achieve this with statistically significant results.6 Subsequent face-to-face courses on the UK integrated clinical academic pathway have produced similar results, reaffirming how an informative course can increase students’ knowledge and preparedness.12
With fears of the decline of academic medicine,3,17 our webinar was focused on providing insight into the application process for a clinical academic career and encouraging students to engage in academia. A survey conducted by Griffin et al.18 found that only 22% of UK medical students had received teaching on writing a research manuscript and a further 62% felt they were not encouraged to participate in research. However, the results of this survey may not be generalisable as the study by Griffin et al.18 was only conducted in seven UK medical schools. Our pre-webinar survey found that 92.3% of attendees had received minimal to no information from their medical school about clinical academic training. Studies in junior doctors have found that feeling well informed about academic careers was statistically linked to an increased desire to continue in academia.19 This reaffirms the idea of institutional disparity if not all students access information about academic careers.12 Initiatives such as this webinar can bridge this gap and give motivated students greater access to the knowledge.
Research conducted by Sura et al.20 explored the use of a focused webinar series to inform medical students about the application for residency in radiation oncology. However, their data collection focused on participants’ characteristics and their concerns. While the authors received ‘positive feedback … and multiple emails with unsolicited favorable comments’, there were no data collected on the webinar’s efficacy to achieve its aims. Whereas our results found that students’ self-rated knowledge and confidence in the AFP application process increased.
Other studies have also reported significant increases in participants’ self-rated knowledge and confidence post-webinar, highlighting that webinars can be an effective teaching platform for both clinical21,22 and nonclinical23–25 education. Mayorga et al.21 explored webinars to improve the learning experience of medical residents. Similarly, Martin et al.25 explored the use of webinars in teaching a systematic approach to medical research. Their study found that 86% of participants were satisfied with the webinar.
As webinars require minimal infrastructure, they have been shown to be cost effective for institutions and participants.14 Of our attendees, 71.2% (84) strongly agreed and 20.3% (24) agreed that webinars offer flexibility and convenience. With barriers of cost and distance minimised, webinars might be considered as a tool in widening access to medical education.
Whilst we identified increases in self-rated knowledge and confidence, there was no statistically significant difference in the interest of attendees in the AFP. We suggest that this is because students willing to attend a webinar on their own volition are already likely to be interested in applying for the AFP. While webinars can reach wider audiences, factors such as marketing, and the self-motivation and preconceived ideas of potential attendees play a role in attendance.
The acceptability of webinars may be attributed to generational differences in learning. Currently, most medical students and junior doctors are millennials. Millennials have been exposed to technology their entire lives and have adapted to function in an environment enhanced by multimedia.26 Studies suggest they prefer Internet resources to textbooks for learning. While they like structured learning and clear objectives, studies have shown millennials prefer information to be provided via available technology.21,27–29 Data from our cohort of millennials did not wholly support this. The median age of participants was 22 years old, only 32.2% (38) of attendees stated that they preferred a webinar to a face-to-face tutorial or lecture and the majority 53.4% (63) stated they had no preference. This might suggest that with the multimedia world of millennials, modern media should be used alongside traditional ‘face-to-face’ teaching. Our findings are supported by the paedological approach popularised by Bergmann et al.,30 they coined the term ‘flipped-classroom’ that believes that lower-order thinking, e.g. comprehension of material and acquisition of knowledge, can be achieved by self-directed learning. This allows precious classroom time to be devoted to completing high-order cognitive tasks.30
While many attendees stated they did not have a preference, a potential advantage of webinars is the increased sense of connectivity. Siemens31 argues that ‘nurturing and maintaining connections is needed to facilitate continual learning’. Webinars allow students to more easily ask questions in real time, removing any barriers caused by shyness. In our study, 68.8% (44) were more likely to ask questions in a webinar than in a live lecture. Participants might be prompted to think differently about a problem as a result of the stream of comments submitted by their peers. Locatis et al.32 found students in webcast conditions rated the instructor significantly higher than those in videoconferencing conditions. This was owing to the fact that instructors in webcast conditions can encourage further learning, by direct and immediate response to their comments and clear misconceptions.
Inherent to cross-sectional studies, a limitation of our study is the small sample size. However, this compares well to what has been reported in similar recent studies, we believe the data is generalisable and, therefore, can be deemed acceptable to yield relevant and significant results.33–36 Moreover, we had representation from 21 of the 41 UK medical schools.37 There may be selection bias as a result of our attendees already having an interest in clinical academia. However, we made sure the webinar was accessible to all UK medical students at no cost.
Further work needs to be carried out exploring if these webinars can enhance student engagement and recruitment into clinical academia in the long term. This could be achieved with a follow-up study of the webinar attendees to investigate their subsequent involvement in academia, not only the success of their AFP application, but assessing their academic outputs.
References
1 Kingston O, Behjati S. Academic medicine. BMJ 2008; 336: s172-s.
2 Academic Careers Sub-Committee of Modernising Medical Careers and the UK Clinical Research Collaboration. Medically- and dentally-qualified academic staff: Recommendations for training the researchers and educators of the future. London: Modernising Medical Careers; 2005. http://www.ukcrc.org/wp-content/uploads/2014/03/Medically_and_Dentally-qualified_Academic_Staff_Report.pdf (accessed 08/07/19).
3 Sheridan DJ. Reversing the decline of academic medicine in Europe. Lancet 2006; 367: 1698–701.
4 Bhutta Z. Practising just medicine in an unjust world. Br Med J (Clin Res Ed) 2003; 327: 1000–1.
5 Ologunde R, Di Salvo I, Khajuria A. The CanMEDS scholar: the neglected competency in tomorrow’s doctors. Adv Med Educ Pract 2014; 5: 383–4.
6 Khajuria A, Cheng K, Levy J. Effect of a national focused course on academic medicine for UK candidates applying for a Clinical Academic Programme. J R Coll Physicians Edinb 2017; 47: 65–9.
7 The UK Foundation Programme Office. Rough Guide to the Academic Foundation Programme. London: The UK Foundation Programme Office; 2013. http://www.foundationprogramme.nhs.uk/sites/default/files/2018-08/Rough%20Guide%20to%20the%20Academic%20Foundation%20Programme.pdf (accessed 08/07/2019).
8 Borrelli MR, Farwana R, Gundogan B et al. How to apply for the academic foundation programme. Ann Med Surg (Lond) 2018; 29: 5–10.
9 Currie GP, Messeder S, Walker K. The Scottish Academic Foundation Year Programme: what, why and how? J R Coll Physicians Edinb 2018; 48: 50–3.
10 The UK Foundation Programme Office. 2019 Recruitment Stats and Facts Report. London: The UK Foundation Programme Office; 2018. http://www.foundationprogramme.nhs.uk/sites/default/files/2018-07/2018%20Recruitment%20Stats%20and%20Facts%20Report%20V2_0.pdf (accessed 08/07/19).
11 Health Careers NHS. Academic Foundation Programme. 2019. https://www.healthcareers.nhs.uk/explore-roles/doctors/career-opportunities-doctors/clinical-academic-medicine/academic-foundation-programme (accessed 08/07/19).
12 Mashar M, Kilgour J, Nanapragasam H et al. Academic medicine: the continuing challenges. Clin Teach 2019 [Epub ahead of print].
13 Wang S-K, Hsu H-Y. Use of the webinar tool (Elluminate) to support training: the effects of webinar-learning implementation from student-trainers’ perspective. J Interactive Online Learn 2008; 7: 175–94.
14 Power M, St-Jacques A. The graduate virtual classroom webinar: A collaborative and constructivist online teaching strategy. J Online Learn Teach 2014; 10: 681.
15 The Royal College of Surgeons of Edinburgh. Webinars. 2019. https://www.rcsed.ac.uk/professional-support-development-resources/learning-resources/webinars (accessed 08/07/19).
16 The Royal College of Surgeons of England. Webinars. 2018. https://www.rcseng.ac.uk/news-and-events/events/webinars/ (accessed 08/07/19).
17 Matthys J. The decline of academic medicine. Lancet 2006; 368: 284–5.
18 Griffin MF, Hindocha S. Publication practices of medical students at British medical schools: experience, attitudes and barriers to publish. Med Teach 2011; 33: e1–8.
19 Lyons OT, Smith C, Winston JS et al. Impact of UK academic foundation programmes on aspirations to pursue a career in academia. Med Ed 2010; 44: 996–1005.
20 Sura K, Lischalk JW, Leckie J et al. Applying for radiation oncology residency: webinar-based medical student mentorship outreach. Int J Radiat Oncol Biol Phys 2017; 97: 11–2.
21 Mayorga EP, Bekerman JG, Palis AG. Webinar software: a tool for developing more effective lectures (online or in-person). Middle East Afr J Ophthalmol 2015; 21: 133–7.
22 Williams JM, Poulsen R, Chaguturu V et al. Evaluation of an online residency training in tobacco use disorder. Am J Addict 2019; 28: 277–84.
23 Martin-Smith JD, McArdle A, Carroll SM et al. Webinar: a useful tool in plastic surgery specialty trainee education. J Plast Reconstr Aesthet Surg 2015; 68: 1423–4.
24 Kumar V, Szeto H, Lehrman ED et al. Expanding the teaching toolbox: characterizing utility of a web-based lecture series in educating future colleagues and referrers about the field of IR. J Vasc Interv Radiol 2019; 30: 589–93.e3.
25 Martin SK, Ahn J, Farnan JM et al. Introduction to curriculum development and medical education scholarship for resident trainees: a webinar series. MedEdPORTAL 2016; 12: 10454.
26 Frand JL. The information-age mindset. Changes in students and implications for higher education. Educause 2000; 15–24.
27 Feiertag J, Berge Z. Training Generation N: how educators should approach the Net Generation. Education Training 2008; 6: 457–64.
28 Moreno-Walton L, Brunett P, Akhtar S et al. Teaching across the generation gap: a consensus from the Council of Emergency Medicine Residency Directors 2009 Academic Assembly. Acad Emerg Med 2009; 16 Suppl 2: S19–24.
29 Mohr NM, Moreno-Walton L, Mills AM et al. Generational influences in academic emergency medicine: teaching and learning, mentoring, and technology (part I). Acad Emerg Med 2011; 18: 190–9.
30 Bergmann J, Sams A. Flip Your Classroom: Reach Every Student In Every Class Every Day: International Society For Technology In Education. USA: International Society for Technology in Education; 2012.
31 Siemens G. Connectivism: A Learning Theory for the Digital Age. 2008. p. 3–10.
32 Locatis C, Berner ES, Hammack G et al. Communication and proximity effects on outcomes attributable to sense of presence in distance bioinformatics education. BMC Med Educ 2011; 11: 10.
33 Nicastro E, Lo Vecchio A, Liguoro I et al. The impact of e-learning on adherence to guidelines for acute gastroenteritis: a single-arm intervention study. PLoS One 2015; 10: e0132313.
34 Knipfer C, Wagner F, Knipfer K et al. Learners’ acceptance of a webinar for continuing medical education. Int J Clin Oral Maxillofac Surg 2019; 48: 841–6.
35 Wagner F, Knipfer C, Holzinger D et al. Webinars for continuing education in oral and maxillofacial surgery: the Austrian experience. J Craniomaxillofac Surg 2019; 47: 537–41.
36 Buxton E, De Muth J. Adult learners’ perceptions of a professional development program comparing live distance learning versus live local learning. J Cont Higher Ed 2012; 60: 12–9.
37 Medical Schools Council. Medical Schools A-Z. 2018. https://www.medschools.ac.uk/studying-medicine/medical-schools (accessed 08/07/19).