Physicians' Gallery Newsletter
Updates on upcoming events, exhibitions and online stories
Scotland's oldest and largest medical library
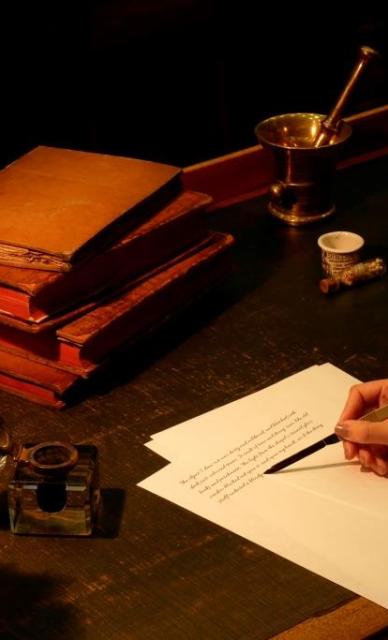
The College library was established in 1682 when our founder, Sir Robert Sibbald, donated “three shelfes full of books to the Colledge of Physitians". It was the first library in Scotland specifically intended for the study of medicine.
We hold over 70,000 books, including a copy of the first edition of the first book printed on medicine - the De Medicina of Celsus, published in 1478 - and almost 1500 journals, some of which are particularly rare.
We also hold over 400 externally deposited manuscript collections concerning eminent scientists such as Joseph Black and William Cullen.
Click on the links below to find out more about our collections and visiting us.
Updates on upcoming events, exhibitions and online stories